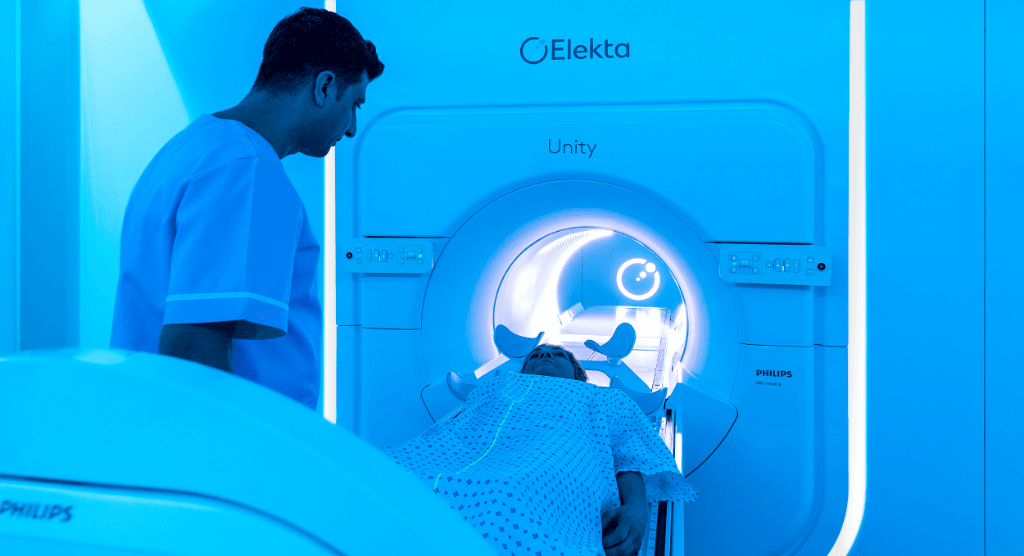
Elekta Unity MR-Linac at home in a small radiotherapy department

Hôpital Riviera-Chablais leverages RTT staff for efficient MR-Linac service

Access to sophisticated radiation therapy technology is often associated with large medical centers, their correspondingly large radiotherapy departments employing dozens of professionals, including radiation oncologists, physicists, dosimetrists and radiotherapy technologists (RTT). The Elekta Unity MR-Linac is an example of an advanced radiotherapy solution that has found its home in places like these. Two years ago, however, the radiotherapy department staff at Hôpital Riviera-Chablais – located in the tiny hamlet of Rennaz, Switzerland (pop. 892 in 2020) – began treating patients with Elekta Unity. The hospital’s experience demonstrates that – with properly motivated and skilled professionals – even smaller departments can successfully use one of the world’s most advanced radiotherapy system.
Marking the second anniversary of their first Unity patient treatment in January 2020, Hôpital Riviera-Chablais medical physicist Marc Pachoud, PhD, radiation oncologist Shaima El Chammah, MD, and RTT Benjamin Jankovic reflect on the implementation and use of their MR-Linac.
Opening just eight years ago, Hôpital Riviera-Chablais began treating patients with its Versa HD™ system, arguably among the most innovative conventional linear accelerator on the market. Equipped with 4D image guidance, High Dose Rate mode (FFF) and high-speed, high-resolution beam shaping, Versa HD has served as an exceptional platform for most of the medical center’s cases and is used for about 45 patient treatments each day. According to Dr. Pachoud, however, the clinical advantages of MR-guided radiotherapy were too attractive to pass up.
“We wanted to be at the top of our radiotherapy capabilities, so we began in 2018 to explore acquiring Elekta Unity.”
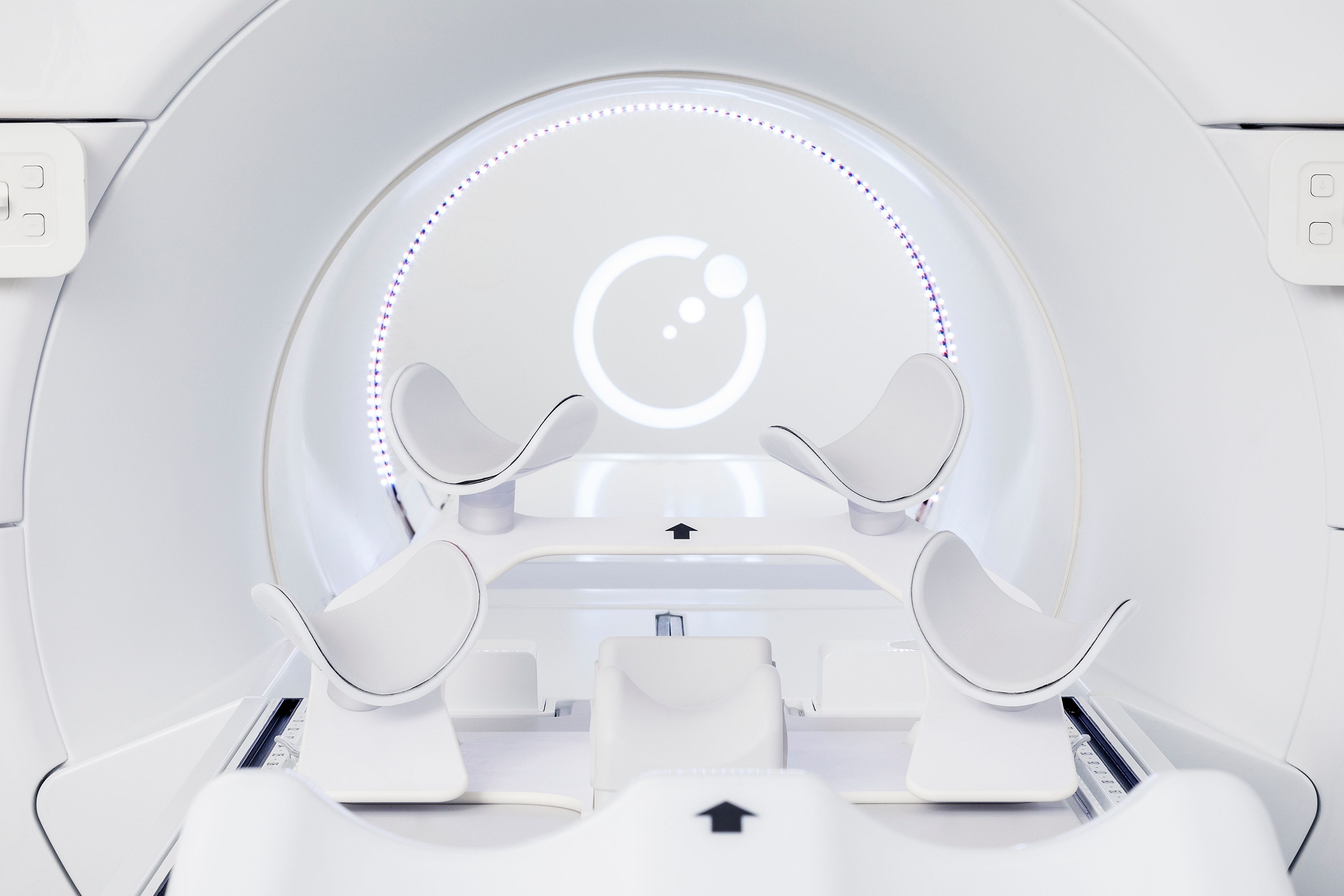
“About 30 percent of the tumors we’re treating are in the pelvic area, such as the prostate and pelvic lymph nodes. We thought that MRI could provide much better image quality to more easily visualize these targets, as well as OARs like the rectum and bowel,” he says. “Moreover, the ability to image during beam delivery would enhance our capacity to perform adaptive treatments, since the prostate and bowel are prone to significant intra-fraction motion. We wanted to be at the top of our radiotherapy capabilities, so we began in 2018 to explore acquiring Elekta Unity.”
Initial doubts give way to confidence
A presentation that Dr. Pachoud heard at an Elekta MR-Linac Consortium meeting gave him the impression that the Elekta Unity workflow was labor-intensive, requiring a crowd of professionals.
“The talk was from one of the larger Unity users,” he recalls. “They had a physicist, two RTTs, a radiation oncologist and a couple others – for a total of six – in the control room to manage the system. That was intimidating for us at first, because we don’t have the staff numbers to make that work.”
A subsequent visit with his colleagues to University Hospital Tübingen’s Unity service gave Dr. Pachoud more insight on how to organize his team and manage the Unity workflow with the department’s limited staff.

“Our main concern was establishing a workflow that worked for the RTTs, the radiation oncologist, the physicist and especially the patient,” Dr. El Chammah says. “At first, we were convinced that a medical presence was necessary during all treatments. But we realized that doesn’t need to be the case in certain situations.”
“At some point, we gained confidence that with greater reliance on our RTTs we could manage the workflow,” Dr. Pachoud adds.
Hôpital Riviera-Chablais decided to acquire Elekta Unity and by December 2019 were ready for onsite training on the installed MR-Linac. In a two-week period, Elekta personnel trained the radiation oncologists, RTTs and physicists, in addition to the nurse and secretary.
RTTs one step ahead
In two critical ways, the hospital’s eight RTTs have been instrumental in the success of the Unity service. First, Hôpital Riviera-Chablais RTT Ben Jankovic and his peers had been doing the dosimetry and OAR contouring on their Versa HD for years. And second, most of the RTTs also had learned about MRI (safety, image interpretation) during undergraduate RTT training.
“The main challenge was getting used to using Monaco for contouring,” he says. “Other than that, during our two weeks of training we had to adjust to the concept that we don’t index the table to adapt the treatment during a Unity session, we move the plan.”
From Dr. Pachoud’s perspective, the trickiest aspect was how to ascertain the Unity reference dose in a magnetic field.
“We spent a lot of time trying to understand this part to ensure we did not miss any correction factor due to the magnetic field,” he recalls. “But concerning the machine itself, it was not a big deal, because there is just one energy. It was quite simple to implement all the QA.”
Crowded control room
While their training instilled confidence in their ability to operate Unity, the Hôpital Riviera-Chablais team still erred on the side of involving many professionals in the workflow at clinical go-live.
“At the beginning, there were two RTTs, a physicist and a radiation oncologist in the control room.”
“At the beginning, there were two RTTs, a physicist and a radiation oncologist in the control room,” Dr. Pachoud observes. “After two weeks, we realized that we could optimize the staffing, so we decided to adopt a more RTT-led service.”
In this workflow, the RTT is responsible for a patient setup, image acquisition and recontouring organs-at-risk. The radiation oncologist is called only to validate the fusion if there is some uncertainty about the automatic fusion. Then, once the plan is ready, the RTT calls the physicist and the plan is validated by both the radiation oncologist (if called upon) and the physicist. Once this is done, the radiation oncologist and physicist leave and the RTT delivers the treatment. If not required to validate the fusion, then the radiation oncologist usually only comes at the end of the process to validate the plan of the day.

“If I am unsure about the fusion, I just carry out the treatment as we RTTs do with Versa HD treatments,” Jankovic explains. “In some cases when the RTT has some doubts about the fusion, he asks for help and decides with the doctor by his side which workflow they want to go through. If the radiation oncologist decides to do adapt-to-shape, he or she just redraws the CTV and I continue with the organs-at-risk and the plan adaptation.”
“In the future, the physician will only be called in if there’s an issue with the fusion or the plan,” Dr. El Chammah adds. “The same will probably be implemented for the physicist. We’re really lucky in our center. We have really excellent RTTs who are very motivated and very competent. When they do call us, it means there’s something unusual to address.”
At home in any center
With its RTT-led workflow firmly established, Hôpital Riviera-Chablais manages to efficiently treat eight to 10 patients on Unity each day. Since the center went clinical with Unity two years ago, it has treated 283 patients, including those with prostate cancer (full-course or hypofractioned) and patients needing boost treatments for anal, rectal or breast cancer.
“Based on our experience, I would say that any center can acquire Elekta Unity.”

“Based on our experience, I would say that any center can acquire Elekta Unity,” Dr. Pachoud says. “It’s just a question of the motivation of the staff and the department’s philosophy. Our department is small, but we decided we wanted to be at the top. I welcome anyone who’s interested in how we have accomplished this to visit our site because seeing is believing.”
The notion that to operate Elekta Unity requires a constant medical presence the entire day turned out to be unfounded, according to Dr. El Chammah.
“You just need to have an RO on call who can come in if needed,” she says. “Once you grasp that and you’re unconcerned about leaving the RTT alone in the control room, then you’ve solved the most daunting issue with this machine.”
“We’re looking forward to studying the feasibility of using Unity for new indications, like head-and-neck cancers, in our department.”
“It has been a good two years with Unity,” Jankovic adds. “We’re looking forward to studying the feasibility of using Unity for new indications, like head-and-neck cancers, in our department.”