Gamma Knife® radiosurgery for medically intractable epilepsy
Case: Medically intractable epilepsy
Author: Professor Dr. R. Martinez, Head of Functional Neurosurgery and Radiosurgery, Ruber International Hospital, Madrid, Spain.
Overview
Epilepsy is a chronic neurological disorder that affects around 50 million people globally1 and is characterized by recurrent seizures. Up to 70% of cases are controlled with antiseizure medications but around 30% have medically intractable epilepsy.1 For these patients, their condition can lead to a poor quality of life and difficulties in undertaking normal daily activities.2
Surgical techniques, including stereotactic radiosurgery (SRS), may be used to improve seizure control and quality of life for medically intractable epilepsy patients.3 Among the known causes for epilepsy that are responsive to surgical intervention are mesial temporal lobe epilepsy (MTLE)4-7 and hypothalamic hamartomas (HHs).4,8,9 In addition, for some patients suffering from complex epilepsies, palliative procedures such as callosotomy can be applied.10
Leksell Gamma Knife® (LGK) SRS, targeting the medial temporal lobe, is a minimally invasive treatment option for MTLE patients contraindicated for, or reluctant to undergo, open surgery,11 offering improved quality of life and protection of cognitive function.4,12 In addition, LGK SRS targeting the HH lesion is an established, safe and effective treatment for medically intractable epilepsy associated with small HHs.9,13-15 It has also been used to treat cases of extra-temporal epilepsy and for palliative procedures, such as anterior corpus callosotomy.10,16
At the Functional Neurosurgery and Radiosurgery Unit at Ruber International Hospital, we have treated 65 medically intractable epilepsy patients using LGK SRS since 1998. Patients with temporal or extratemporal epilepsy (60% male, 40% female) ranged from 25-36 years old (median 27 years). Patients with HH (55% female, 45% male) ranged from 1.5-45 years old (median 18 years). These patients experienced daily, very disabling epileptic seizures that did not respond to medication. Most had an epileptic history of at least 7 years, except for severe cases of HH in childhood where we acted immediately due to the severity of the condition. Around 75% of patients could not lead an active life due to their condition. In addition to epileptic seizures, major symptoms prior to LGK SRS included cognitive impairment and aggression.
Our experience of treating epileptic patients with callosotomy is more limited. We have performed this procedure in five patients aged between 16 and 25 years.
In all cases, LGK SRS was selected due to potential surgical risk, including post-surgery neurological deficit, and according to patient choice.
Radiosurgical Protocol
Our inclusion criteria for this study are as follows:
- A confirmed diagnosis of MTLE, extratemporal epilepsy or HH based on high-resolution MRI findings.
- Refractory epilepsy that failed to respond to standard anti-epileptic drugs.
- Availability of longitudinal clinical and radiological follow-up data.
Prior to 2018, patients were fitted with the Leksell G type stereotactic frame and, since 2018, they have been immobilized using the Leksell Vantage™ frame. Patients under 12 years of age, and those with significant behavioral problems, are treated under general anesthesia. Otherwise, light sedation and control of epileptic seizures have been sufficient to deliver treatments without problems.
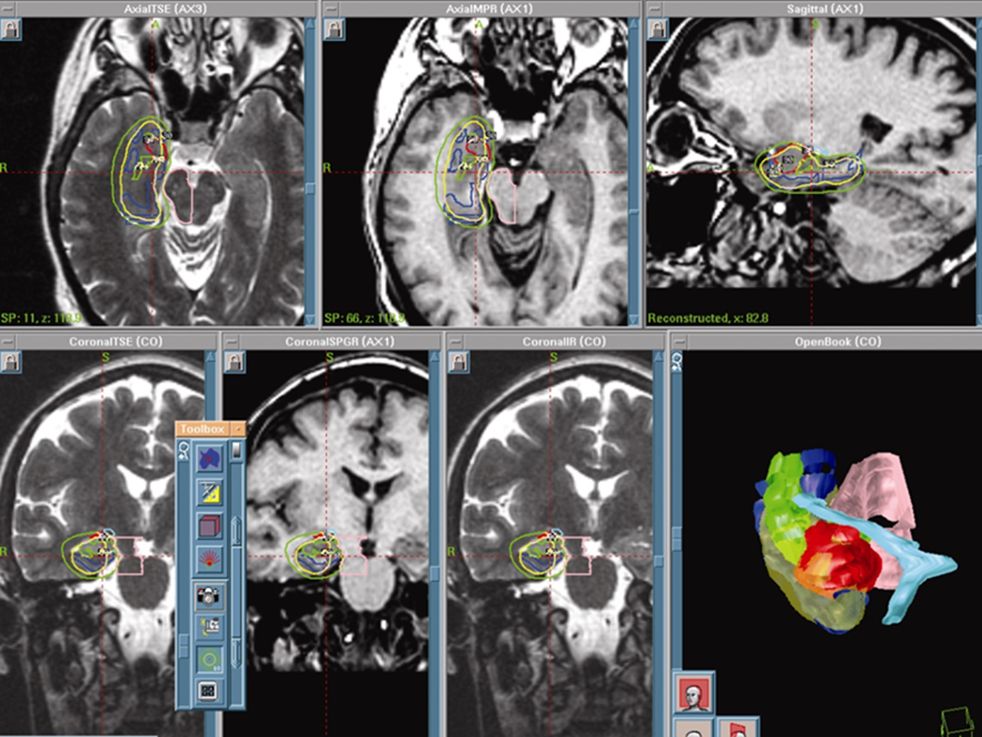
Pre-treatment imaging includes high-resolution T1- and T2-weighted MRI with 1–1.5 mm slices of the whole brain, incorporating contrast enhancement with the T1 series. Planning is carried out using Leksell GammaPlan® treatment planning software.
The radiosurgery is performed using the Leksell Gamma Knife, (Gamma Knife versions B and C prior to 2007, Gamma Knife Perfexion from 2007-2017, and Gamma Knife Icon since 2017).
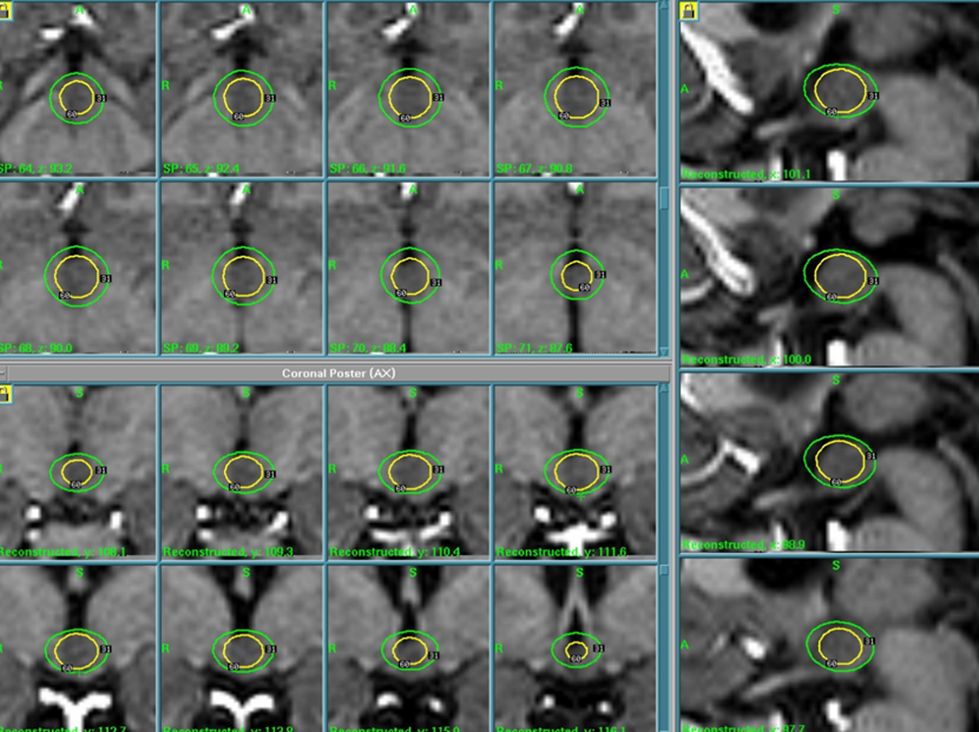
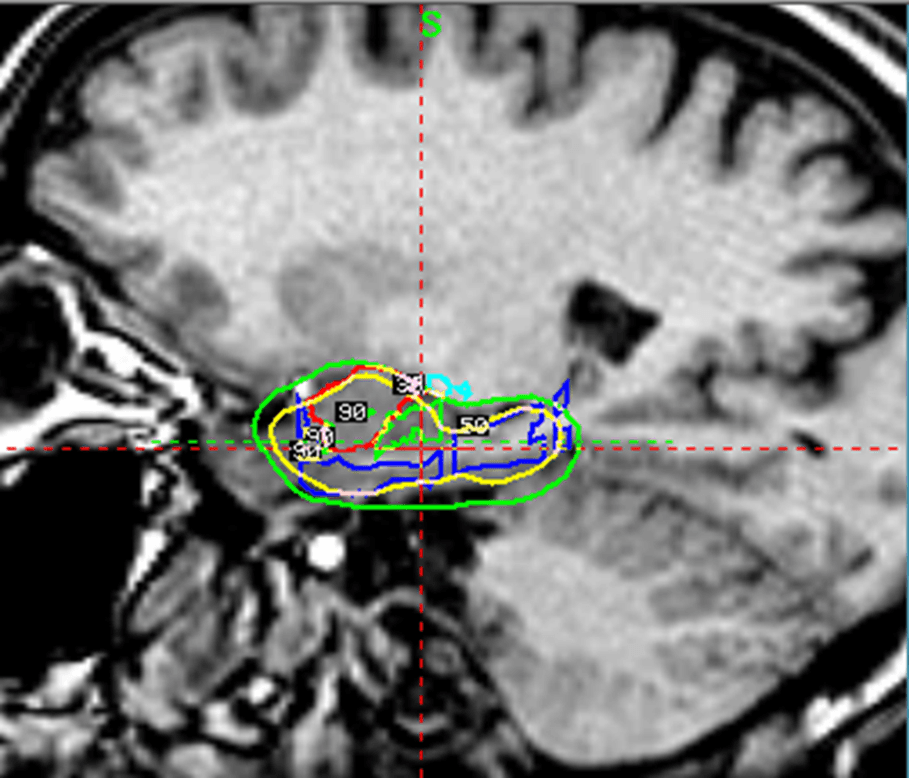
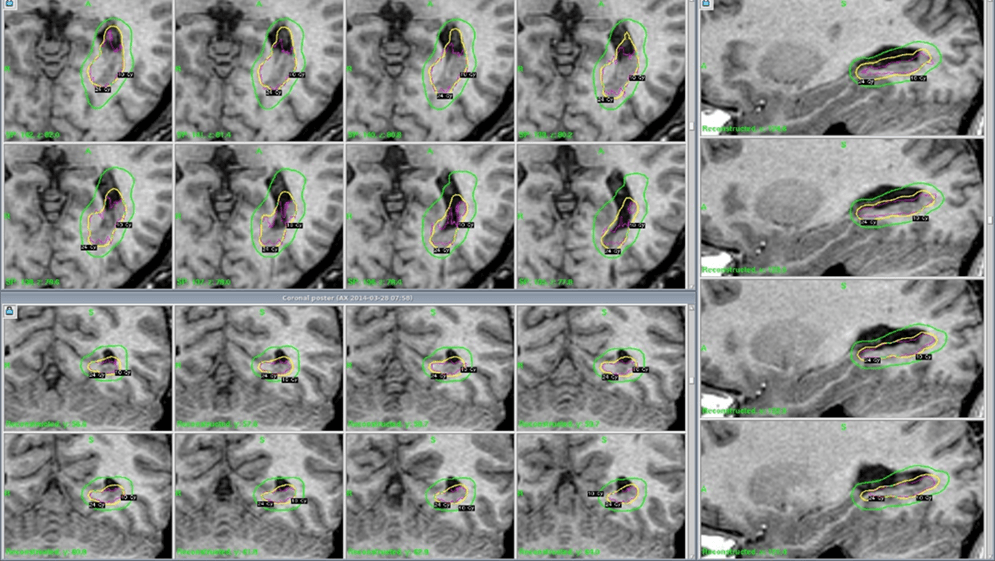
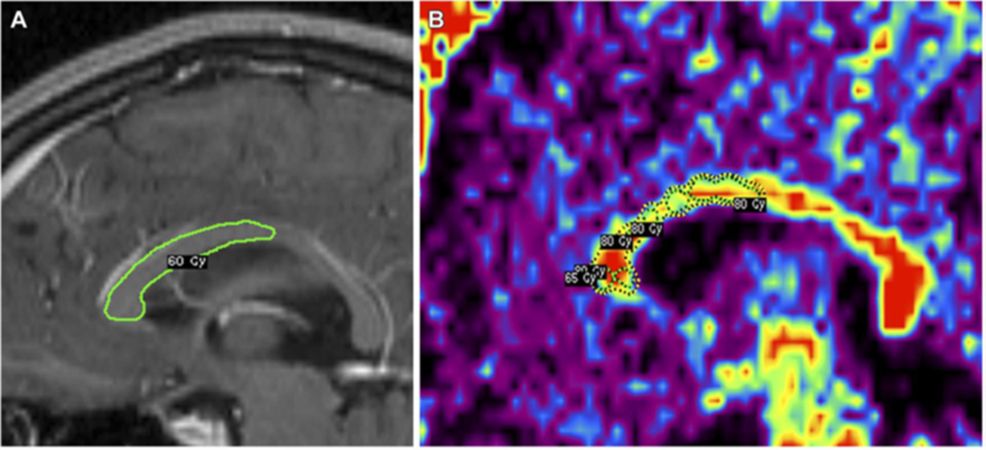
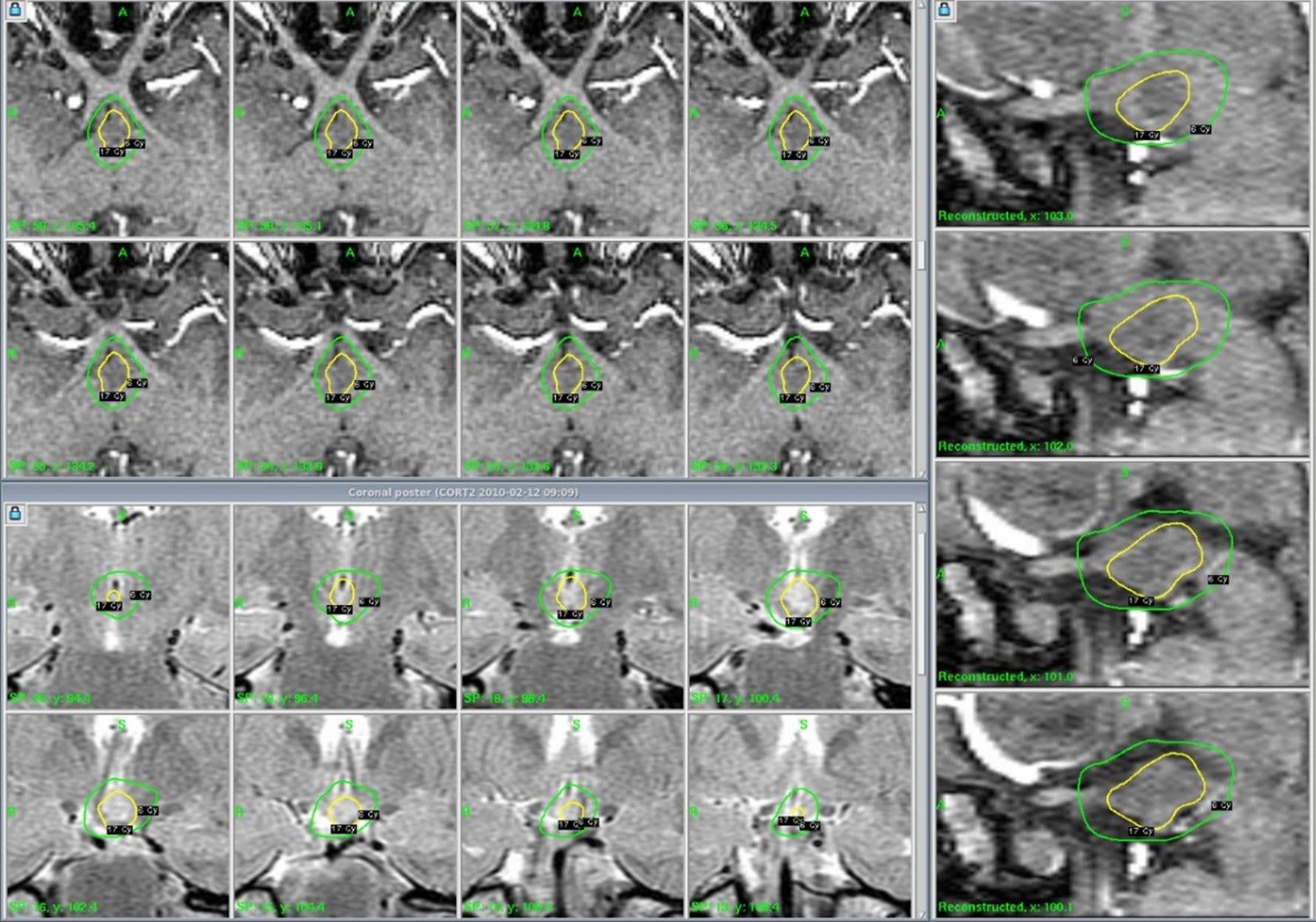
For HHs, the treatment plan aims to encompass the entire lesion, with a median marginal dose of 16–20 Gy delivered to the 50% isodose line (figures 1 and 2). For MTLE, the target volume includes the hippocampus, amygdala, and parahippocampal gyrus, with a prescription dose of between 24–25 Gy at 50% isodose (figures 3 and 4). For extratemporal epilepsy, the target is determined by prior stereoelectroencephalography (SEEG) and planning is adapted in GammaPlan using MRI under stereotaxic conditions (figure 5). The target volume includes the cortex of the epileptic focus with the same dose and isodose parameters applied in MTLE.
Risk areas at the target periphery include the brainstem, optic pathway and hypothalamus. The maximum dose to these structures is kept to less than 10 Gy.
In callosotomy procedures, we target specific regions of the corpus callosum to disrupt interhemispheric seizure propagation, especially in the anterior (figure 6). The maximum dose applied is 120 Gy, with a coverage dose of 60 Gy at the 50% isodose. The volume of peripheral brain tissue that receives more than 10 Gy has always been less than 3 cm3.
These Gamma Knife treatments last between 1-3 hours. Afterwards, patients remain under observation for 4 hours before they are discharged. They do not require additional medication and must remain on anti-epileptic treatment. Patients tolerate the treatment extremely well with no immediate side effects. Follow-up consists of consultations and MRI scans every six months for the first 3 years, and then annually for at least another 5 years.

Results
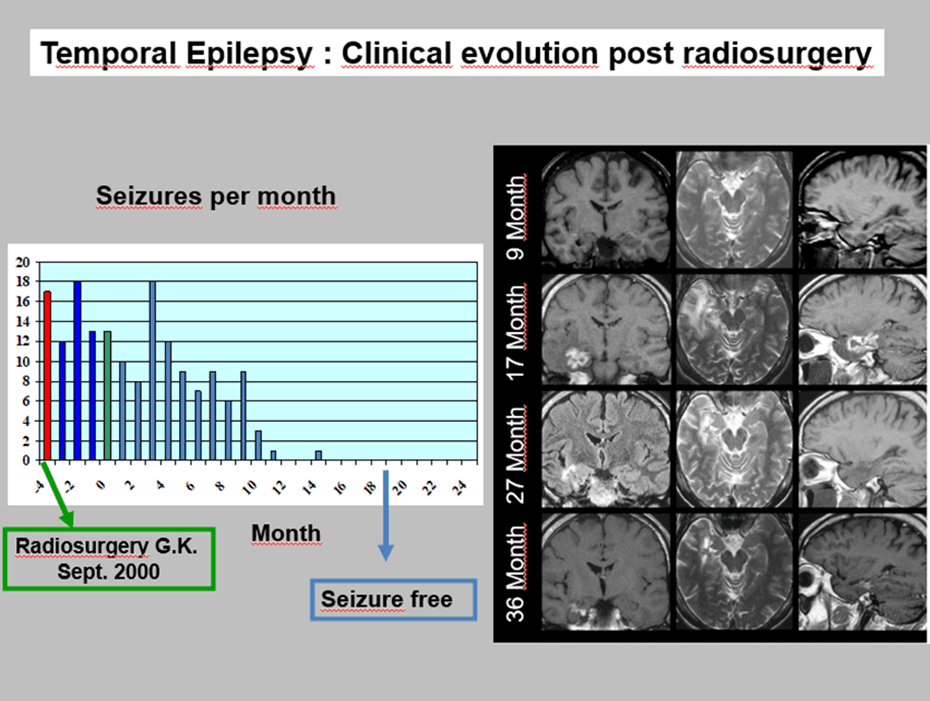
The overall response for the treatment of medically intractable epilepsy using LGK SRS at our institution is 70% (to Engel I or II* with or without mediation) in cases of HH, MTLE and extratemporal epilepsy.
After LGK callosotomy, drop attacks have been controlled in four out of five patients treated. General seizures have decreased in severity and frequency in all callosotomy patients, but they remain at Engel III.
In all cases, there were no permanent side effects, although transitory depression was experienced in two cases of MTLE.
LGK SRS has a significant impact on patient quality of life, which improved, on average, by 70% on quality-of-life measurement scales (EQ-5D health states17). At least 70% of cases are able to work normally and, in cases of HH, 90% have improved with respect to behavior and cognitive deficit.
In 50% of HH cases, we observed a reduction in the HH volume (figure 7). 30% of cases were treated again due to exacerbation of the crises. These patients improved again after the second treatment.
In cases of MTLE, the effects of LGK SRS increased over time, reaching its full effect 12 months post-radiosurgery. All cases showed some degree of long-term mesial temporal atrophy after treatment (figure 8).
Discussion
Radiosurgery, particularly LGK SRS, has emerged as a minimally invasive alternative for treating certain forms of drug-resistant epilepsy. The reviewed literature evaluates its safety, efficacy, and broader impact on patient outcomes across different types of epilepsy, including corpus callosotomy for refractory seizures, HHs, and focal epilepsies.18-22 Radiosurgery impacts the epileptogenic zone by inducing delayed necrosis and neuromodulation19, gradually reducing seizure activity over months.
Systematic review of radiosurgery in epilepsy applications demonstrates the use of radiosurgery to treat MTLE,5-7,12 extratemporal epilepsy,16 HH13-15 and for callosotomy.10
HH-related epilepsy often presents as gelastic seizures, which may progress to catastrophic epileptic encephalopathy. Radiosurgery offers a non-invasive alternative to traditional resective surgery. In a prospective trial involving 48 patients, 68.8% achieved Engel Class I/II outcomes, indicating seizure freedom or substantial improvement. Psychiatric comorbidities improved or resolved in 84% of cases. No permanent neurological deficits were reported.13-15
Gamma Knife Corpus Callosotomy (GK-CC) is primarily used for patients with intractable epilepsy characterized by severe drop attacks (DAs) and generalized seizures. In a cohort of 19 patients10, 68% experienced significant seizure reduction and 16% achieved complete seizure freedom. Transient side effects were mild and no major long-term complications were reported. GK-CC demonstrates comparable efficacy to traditional surgical callosotomy2,10 while minimizing risks such as infection, disconnection syndrome, and cerebrospinal fluid leakage.
Level 2 evidence supports radiosurgery in MTLE and HH.18 In other cases, palliative radiosurgery, such as callosotomy, shows promise in reducing seizure burden in inoperable or high-risk cases.
Challenges associated with radiosurgery include delayed therapeutic effects (several months) and the absence of randomized controlled trials limit the establishment of definitive guidelines.12,15,18,19 However, the advantages of radiosurgery over surgery are that it offers reduced risk of permanent deficits and favorable neuropsychological outcomes compared to resective procedures.3,6 Although radiosurgery avoids many risks associated with open procedures, including infection, significant neurological deficits, and prolonged recovery, it requires precise imaging and planning to target the epileptogenic zone effectively6,7.
Looking ahead, randomized trials comparing radiosurgery with conventional surgical techniques are necessary to solidify its role in epilepsy management18. In addition, technological advances, such as improved imaging and targeting methodologies, may further enhance outcomes.
Conclusions
LGK SRS allows us to deliver an extremely precise and accurate radiation dose to epileptic targets within the brain, while sparing the surrounding healthy tissue and critical structures. In our experience, this is a safe and effective treatment option for medically intractable epilepsy, providing a treatment response rate in line with published evidence.4,5,7,10,12,14,18-22
Radiosurgery represents a valuable option for managing specific epilepsy subtypes, particularly for patients unsuitable for traditional surgery. Its safety profile and efficacy justify its inclusion in comprehensive epilepsy treatment strategies.
References
- WHO, Epilepsy Key Facts 2024 https://www.who.int/news-room/fact-sheets/detail/epilepsy#:~:text=The%20estimated%20proportion%20of%20the,diagnosed%20with%20epilepsy%20each%20year
- Sachdev S, Sita TL, Shlobin NA, et al. Completion Corpus Callosotomy with Stereotactic Radiosurgery for Drug-Resistant, Intractable Epilepsy. World Neurosurg. 2020 Nov:143:440-444. doi: 10.1016/j.wneu.2020.08.102. Epub 2020 Aug 20.
- Joris V, Weil AG, Fallah A. Brain Surgery for Medically Intractable Epilepsy. Advances in Pediatrics. August 2022; Volume 69, Issue 1: 59-74
- Yang I, Barbaro NM. Advances in the Radiosurgical Treatment of Epilepsy. Epilepsy Currents. 2007;7(2):31-35. doi:10.1111/j.1535-7511.2007.00160.x2006
- Wang X-Q, Zhang X-D, Han Y-M, et al. Clinical efficacy of gamma knife and surgery treatment of mesial temporal lobe epilepsy and their effects on EF-Tumt and EF-Tsmt expression. Eur Rev Med Pharmacol Sci. 2017 Apr;21(8):1774-1779.
- Marathe K, Alim-Marvasti A, Dahele K, et al. Resective, Ablative and Radiosurgical Interventions for Drug Resistant Mesial Temporal Lobe Epilepsy: Systematic Review and Meta-Analysis of Outcomes. Front. Neurol. 2021;12:777845. doi: 10.3389/fneur.2021.777845
- Régis J, Bartolomei F, Rey M, et al. Gamma knife surgery for mesial temporal lobe epilepsy. Epilepsia. 1999 Nov;40(11):1551-6. doi: 10.1111/j.1528-1157.1999.tb02039.x.
- Wei Z, Vodovotz L, Luy DD, et al. Stereotactic radiosurgery as the initial management option for small-volume hypothalamic hamartomas with intractable epilepsy: a 35-year institutional experience and systematic review. J Neurosurg Pediatr. 2022 Oct 21;31(1):52-60. doi: 10.3171/2022.9.PEDS22200. Print 2023 Jan 1.
- Hamdi H, Albader F, Spatola G, et al. Long-term cognitive outcome after radiosurgery in epileptic hypothalamic hamartomas and review of the literature, Epilepsia. 2021 Jun;62(6):1369-1381. doi: 10.1111/epi.16896. Epub 2021 Apr 20.
- Hamdi H, Boissonneau S, Valton L, et al. Radiosurgical Corpus Callosotomy for Intractable Epilepsy: Retrospective Long-Term Safety and Efficacy Assessment in 19 Patients and Review of the Literature. Neurosurgery. 2023, July; 93 (1): 156-167.
- Barbaro NM, Quigg M, Ward MM et al. Radiosurgery versus open surgery for mesial temporal lobe epilepsy: The randomized, controlled ROSE trial. 14 February 2018; 59: 1198-1207. DOI: 10.1111/epi.14045.
- Régis J, Rey M, Bartolomei F, et al. Gamma knife surgery in mesial temporal lobe epilepsy: a prospective multicenter study. Epilepsia. 2004 May;45(5):504-15. doi: 10.1111/j.0013-9580.2004.07903.x.
- Lu D, Wang T, Yang Y, et al. Advances in hypothalamic hamartoma research over the past 30 years (1992-2021): a bibliometric analysis Front Neurol. 2023 Jun 6:14:1176459. doi: 10.3389/fneur.2023.1176459. eCollection 2023.
- Régis J, Scavarda D, Tamura M, et al. Gamma knife surgery for epilepsy related to hypothalamic hamartomas. Semin Pediatr Neurol. 2007 Jun;14(2):73-9. doi: 10.1016/j.spen.2007.03.005.
- Régis J, Lagmari M, Carron R, et al. Safety and efficacy of Gamma Knife radiosurgery in hypothalamic hamartomas with severe epilepsies: A prospective trial in 48 patients and review of the literature. Epilepsia. 2017 Jun:58 Suppl 2:60-71. doi: 10.1111/epi.13754.
- McGonigal A, Bartolomei F, Gavaret M, et al. Gamma knife radiosurgery of paracentral epilepsy. Stereotact Funct Neurosurg. 2014;92(6):346-53. doi: 10.1159/000364915. Epub 2014 Oct 28.
- Brooks R. EuroQol: the current state of play. Health Policy 1996; 37: 53-72.
- McGonigal A, Sahgal A, De Salles A, et al. Radiosurgery for epilepsy: Systematic review and International Stereotactic Radiosurgery Society (ISRS) practice guideline Epilepsy Res. 2017 Nov:137:123-131. doi: 10.1016/j.eplepsyres.2017.08.016. Epub 2017 Sep 20.
- Régis J. Gamma knife for functional diseases. Neurotherapeutics. 2014 Jul;11(3):583-92. doi: 10.1007/s13311-014-0276-z.
- Lee EM, Kang JK, Kim SJ, et al. Gamma Knife radiosurgery for recurrent or residual seizures after anterior temporal lobectomy in mesial temporal lobe epilepsy patients with hippocampal sclerosis: long-term follow-up results of more than 4 years . J Neurosurg. 2015 Dec;123(6):1375-82. doi: 10.3171/2014.12.JNS141280. Epub 2015 Jul 10.
- Bartolomei F, Hayashi M, Tamura M, et al. Long-term efficacy of gamma knife radiosurgery in mesial temporal lobe epilepsy. Neurology. 2008 May 6;70(19):1658-63. doi: 10.1212/01.wnl.0000294326.05118.d8. Epub 2008 Apr 9.
- Abla AA, Shetter AG, Chang SW, et al. Gamma Knife surgery for hypothalamic hamartomas and epilepsy: patient selection and outcomes. J Neurosurg. 2010 Dec:113 Suppl:207-14. doi: 10.3171/2010.8.GKS101027.
*According to the Engel Classification Scale for epilepsy surgery outcomes, as follows:
- Class I: Free of disabling seizures
- Class II: Rare disabling seizures, less than 3 seizure days per year
- Class III: Worthwhile improvement, or greater than 80% reduction in seizure frequency
- Class IV: No worthwhile improvement, or less than 80% reduction in seizure frequency
LGK has U.S. FDA 510(k) clearance for Refractory/pharmaco-resistant/intractable mesial temporal lobe epilepsy (MTLE) in adults, with other countries requiring regulatory approvals to add this indication. It is also cleared for refractory epilepsy associated with structural changes such as hamartomas, cerebral cavernous malformations, and arteriovenous malformations (adult and pediatric)