Upskilling radiographers can help to improve radiotherapy access and tackle the post-lockdown cancer backlog

By Dr Anna Britten, Director of Medical Affairs, Elekta
The COVID-19 pandemic has limited GP access which in turn has impacted the cancer referral pathways. As a result, there are now tens of thousands of patients waiting to be seen, putting more demand on services that are already under pressure.
The spectrum of COVID-19 related harm is wide and includes halting screening and prevention efforts, delaying timely diagnosis and staging of new patients, delaying initiation of therapy, interrupting ongoing treatment, delivering suboptimal palliative care, and disrupting clinical research.
According to figures published in The Lancet, while all cancer treatments were affected (systemic therapies, radiation therapy and surgery), radiation therapy did relatively better than others in that we saw the least reduction in its services (14% fewer treatments compared to 31% in systemic therapies and 29 to 40% in surgery). Nonetheless, figures from the Radiotherapy Dataset show that there were approximately 13,700 fewer radiotherapy patients treated within the nine-month period from April 2020 to January 2021.
A recent European survey similarly found that there was a reduced use of palliative radiotherapy (aimed to provide relief from cancer-related symptoms), as well as reduced treatment of the elderly. In addition, more treatments courses were interrupted, and more curative courses of radiotherapy were given for indications normally treated with surgery. Interestingly, during this time there has also been a small move away from evidence-based radiotherapy protocols to more hypofractionation (and ultra hypofractionation) to compensate for a reduction in surgery and systemic cancer therapy administration.
At an online cancer summit recently, APPG for Radiotherapy chair Tim Farron MP said that those working in cancer services have the expertise needed to tackle the backlog but only if ministers are willing to accept there is a crisis, deliver vital investment in cancer services, and act quickly. A flash survey looking at the impact of COVID-19 on UK radiation therapy one year on, found that, while 91% of respondents felt that it should play a significant/very significant role in reducing the COVID-19 cancer backlog, there were also fears that the service would be unable to cope with the tsunami of cases that would be coming its way.
It stands to reason that, if radiotherapy is to successfully play a part in reducing the backlog, we must create more capacity, allowing better access for those who need it. Recognising the abilities of staff to take on different roles, and upskilling them to take on those extra responsibilities, will assist in accelerating implementation of advanced technologies and quicker, faster, automated workflows. This is where – with human supervision – AI can be used to take over a fair proportion of the radiotherapy workflow, ensuring greater capacity, improving access, enabling a reduction in post-lockdown cancer backlogs and more importantly, allowing staff to spend more time with the patients.
However, in order to successfully implement new technology, professional users need to be appropriately trained. Therefore, education and training is key to modernising and creating sustainability. But this sadly has not taken place in the NHS, where radiotherapy services have been historically overlooked and underfunded with barely 5% of the NHS cancer budget dedicated to all aspect of this technologically complex and life-changing therapy.
A dwindling workforce (exacerbated by the pandemic as burned-out staff review their career choices), combined with a rise in patient numbers, has resulted in a clinically significant NHS-wide under-resourced radiotherapy service. To attempt to bridge that gap, it is crucial to introduce role diversification, whereby radiographers are upskilled to take on more ‘clinical’ responsibilities, such as contouring.
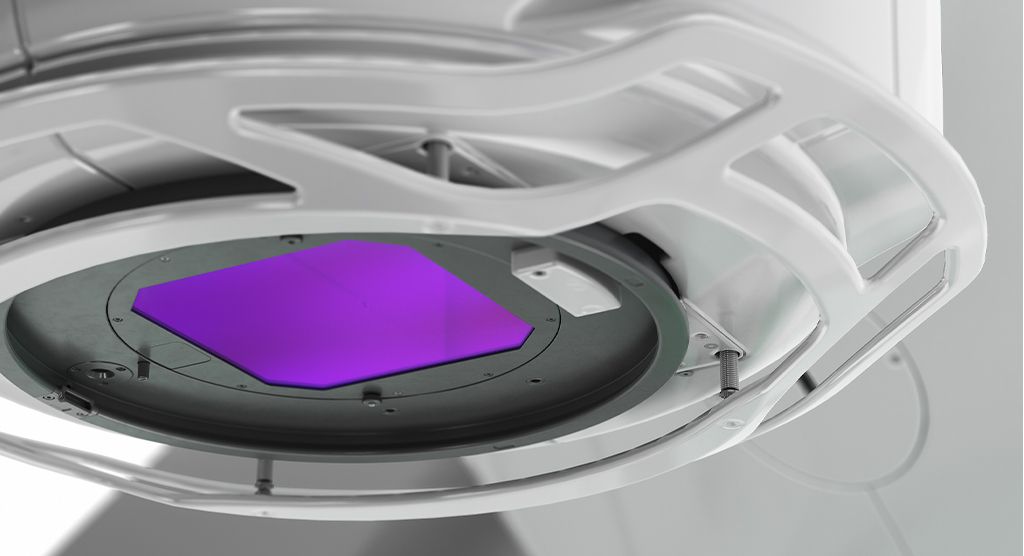
Contouring is a step in the radiotherapy process that is most subjective and therefore prone to weakness in standardisation, but has the unparalleled potential to significantly improve patient outcomes. It entails drawing around the targets needing to be treated accurately, and around the anatomy which needs to be avoided, thereby increasing the accuracy and reducing the side effects.
The COVID-19 pandemic has meant that many radiographers are missing out on education and training, as well as new career progression opportunities. If this is not addressed quickly, there cannot be an expansion of radiotherapy services to address the COVID-19 cancer backlog, nor an introduction of vital radiotherapy innovation, and consequently, no improvement in cancer patient outcomes.
Elekta is focused on supporting and providing training for radiographers and radiation oncologists. Our cloud-based contouring and planning academies (ECA and EPA) provide the training needed to a global workforce dedicated to providing the best cancer care in the midst of a global pandemic.