UK center continues brachytherapy evolution with Elekta’s Venezia applicator
Added “reach” of advanced gynecological applicator benefiting patients with advanced cervical cancer at Royal Surrey County Hospital

Thanks to the UK National Health Service’s extensive screening programs for cervical cancer, the country’s incidence of advanced cases is relatively low—most brachytherapy centers will have a suitable applicator for the majority of cervical cancer patients needing treatment. But for patients whose cancer has spread to the parametrium and beyond, gynecological brachytherapy applicators that enable the placement of interstitial needles are useful in extending the therapeutic dose to reach the disease. Veterans in interstitial brachytherapy, clinicians in Royal Surrey County Hospital’s (RSCH, Guildford, UK) brachytherapy department have recently reinforced their interstitial capabilities with the addition of the Venezia™ Advanced Gynecological Applicator. Clinicians began using Venezia to treat patients in December 2019.

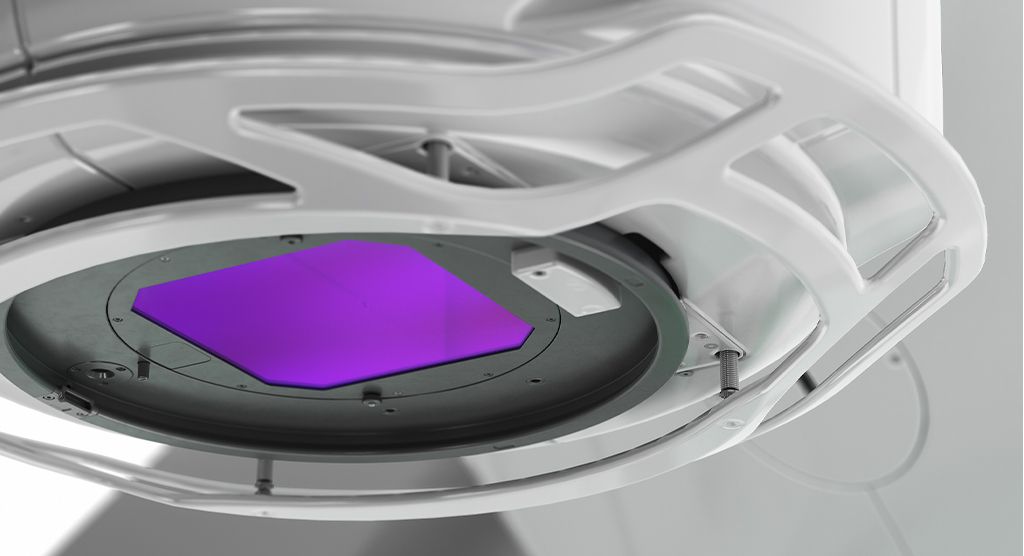
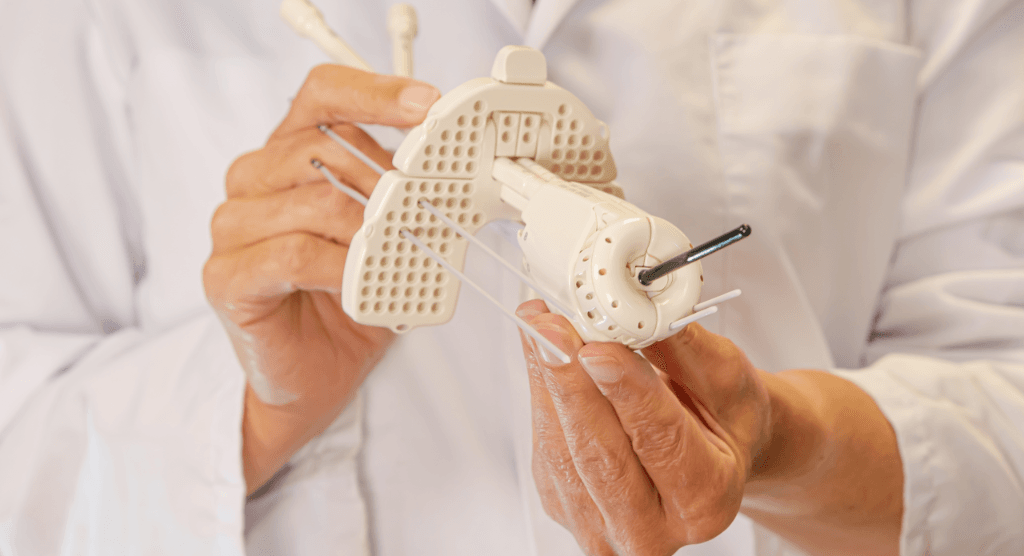
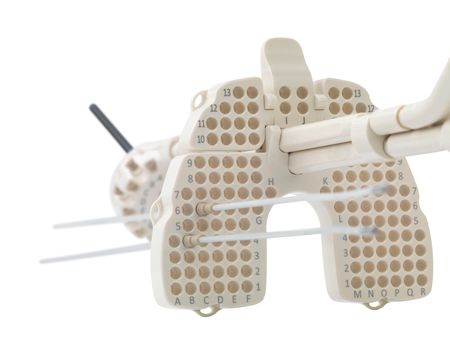
Key features of Venezia include holes in its two lunar ovoids (see photo) for not only parallel needle placement, but also oblique needle placement for pushing the dose out laterally (i.e., pelvic side wall). Venezia also integrates a perineal template for the placement of parallel needles to reach tumor extension anterior and/or lateral to the vagina and cervix, and vaginal caps to treat the lower part of the vaginal wall.
“Before Venezia, we didn’t have an option for interstitial applicator plus perineal template—it was either template interstitial or applicator interstitial,” according to Dr. Alexandra Stewart, RSCH Consultant Clinical Oncologist. “As an experienced brachytherapist, I could often achieve appropriate dose distributions using the Utrecht applicator and free-hand placement of needles—thereby making our own version of adding a template to applicator interstitial brachytherapy.
“However, the holes in the Venezia perineal template enable a much more predictable, reproducible needle path, while the holes in the Venezia ring allow us to obliquely extend the dose past Point A to reach disease spread,” Dr. Stewart adds. “We will continue to use the Utrecht applicator for most cases and reserve Venezia for patients with parametrial invasion, vaginal involvement and disease outside the cervix that needs coverage. We may also use it for vulvar cases and vaginal cancer if there is extension toward the cervix.”
“[T]he holes in the Venezia perineal template enable a much more predictable, reproducible needle path, while the holes in the Venezia ring allow us to obliquely extend the dose past Point A to reach disease spread.”
Venezia debuts at RSCH
RSCH clinicians integrated Venezia into their brachytherapy workflow in December 2019. For the first patient (36-year-old with FIGO 2018 T31r squamous cell carcinoma [previous FIGO stage T2B]), the results of the previous day’s MRI scan indicated the need for interstitial needles. Using the Utrecht applicator initially, the first fraction was delivered with six needles and 25 mm ovoids.

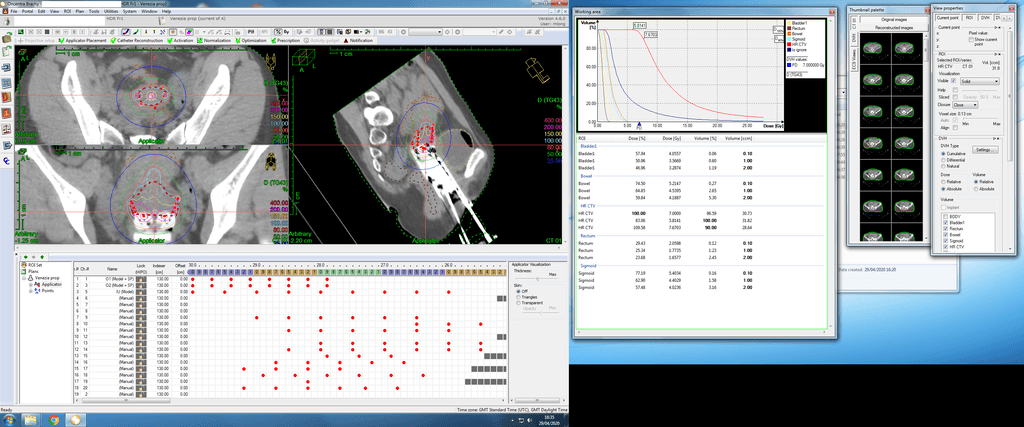
“In our iterative pre-planning technique1, we’ll ask physics if we could have improved the dose distribution if we had used additional interstitial needles,” she explains. “Physics does a post-plan for Fraction 1 and Fraction 2, and they might say, for example, if we had placed a needle in position 7 and advanced it 3 cm, we would have decreased the rectal dose or improved the coverage of the high-risk CTV. So, for every patient we treat, we look to see if we can improve the next fraction by adding needles.”
The first patient’s second fraction again employed the Utrecht applicator using 30 mm ovoids and a total of six needles, two of which were placed free-hand in the parametrium, with transrectal ultrasound guidance. In RSCH’s first use Venezia, Fraction 3 involved the placement of 14 needles (13 used in plan) through 26 mm lunar ovoids.
“The second case in which we used Venezia was a 54-year-old patient with a very bulky T4A tumor with marked bladder and urethral invasion,” Dr. Stewart says. “In this case, we used Venezia for all three fractions and used the applicator’s perineal template for the first time.”
In this case, the first fraction employed 22 mm lunar ovoids (4 perineal needles, 8 needles through ovoids) and the second and third fractions used 22 mm lunar ovoids (2 perineal needles, 7 needles through ovoids).
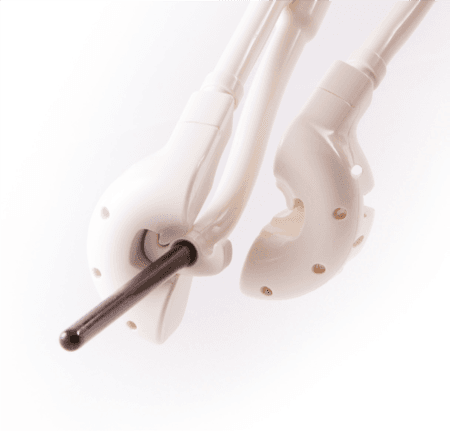
RSCH’s third patient debuted the applicator’s vaginal caps inferior to the ring that accommodate catheters for treating the vaginal wall. The caps simply snap onto the semi-lunar ovoids and insertion is no different than placing the ovoids alone. The patient, who had vaginal/vulvar cancer wrapped around the urethra, involved the use of the vaginal caps with two needles, then the anterior interstitial template with six needles, followed by two free-hand placed needles anterior to the template. She received a total of four fractions.
“Whether patients get interstitial needles or no needles, they are basically treated the same way in terms of their ability to be discharged home,” she notes. “Even the patient treated with Venezia with the perineal template still went home that afternoon.”
Design advantages
Aside from the ability to place parallel and oblique needles, the two lunar-shaped ovoids form a ring that when clicked together provide the ease of insertion of a tandem and ovoid applicator in combination with the dose distribution afforded by a ring applicator. The ring creates a pear-shaped dose distribution, a proven dosimetry shape that matches the cervix and endometrium.
“Venezia is easy to click together at the cervical external os and the availability of a narrower tandem is nice too,” Dr. Stewart observes. “We also purchased both the 22 mm and 26 mm ovoids and we used them both on the first two patients. Selection is based on patient anatomy influenced by factors such as whether the patient had children before or the patient’s age.”
The lunar ovoid design of Venezia also contributed to simpler commissioning versus a conventional ring applicator, according to RSCH physicist Mel Cunningham.
“When we would work to localize the source path of our ring applicators using gafchromic films, it didn’t bear much resemblance to the model of them in the Oncentra Brachy planning system,” Cunningham says. “The reason was you’re sending a source on a cable at speed and driving it around a circle—the source doesn’t always go to the same place consistently. Whereas with the Venezia lunar ovoids, the source only goes up but never over the top; there is no issue of bending a cable around the curve and having different friction.”
A predictable source path is important in planning a treatment that maximally targets the tumor and spares organs-at-risk (OAR), she adds.
“While commissioning Venezia we found that after repeated source path localizations, the source was consistently going to the same place.”
“Oncentra Brachy has an applicator modeling function that allows you to reconstruct the applicator very quickly,” Cunningham explains. “However, if the source is not going precisely to where the planning system thinks it’s going, then when I’m optimizing doses I could actually be overdosing the OARs and underdosing the tumor. While commissioning Venezia we found that after repeated source path localizations, the source was consistently going to the same place. We have become confident that it will be consistent between applicators and between source changes.”
On hand when you need it
Despite the relatively few advanced cervical cancer cases RSCH will see in any given year that would necessitate a solution like Venezia, Dr. Stewart says the acquisition of one or more Venezia applicators is likely.
“We want the availability of Venezia when we need it for the more advanced cases,” Dr. Stewart says. “As we replace and renew our applicators, we’re virtually certain to buy another Venezia, and then probably use it more interchangeably with the Utrecht applicators.
“Applicator interstitials like Venezia allow clinicians to use needles with more confidence, encouraging them to move toward even more interstitial work,” she continues. “What we are trying to do is bring other brachytherapy teams in and teach them how to do it themselves. Although we are happy to treat other centers’ patients if there is no interstitial availability locally, we would prefer that there are cohorts of brachytherapists around the country that are just as confident using interstitial needles as we are.”
Royal Surrey County Hospital cervical cancer brachytherapy protocol
- MR- and CT-guided
- Node positive patients: EBRT (50.4 Gy, 28 fractions), brachytherapy boost (21-28 Gy, 3-4 fractions)
- Node negative: EBRT (45 Gy, 25 fractions), brachytherapy boost (28 Gy, 4 fractions)
- Clinical aim: D90 to high-risk CTV to 90-95 Gy EQD2
- Most patients are ≥ stage 1B2, particularly in 2018 FIGO staging that accounts for positive lymph nodes
- Applicators: Utrecht used initially for nearly every case. If there is middle/lower one-third vaginal invasion a tandem and cylinder applicator was used but now RSCH clinicians will use Venezia for cases with significant parametrial/extension outside cervix/vaginal extension.
- Afterloader: Flexitron
- Typically, clinicians perform single fraction insertions under spinal anesthesia with sedation during insertion. Patients are in the department for approximately four hours and discharged home the same day even after interstitial needle placement. Since Covid-19, patients are offered one insertion with two fractions treated at a 6-hour interval, going home that day or the next morning. Patients have found this very acceptable so it is likely this will be continued after Covid-19 scheduling challenges resolve.
- Department performs 2-3 gynecological brachytherapy implants per week
- Otter S, Franklin A, Ajaz M, Stewart A. Improving the efficiency of image guided brachytherapy in cervical cancer. J Contemp Brachytherapy. 2016;8:557–565. [PMC free article] [PubMed] [Google Scholar]
UK Cervical Cancer Statistics
There are approximately 3,200 new cervical cancer cases in the United Kingdom each year – averaging more than eight every day (2015-2017). Among UK women, cervical cancer is the 14th most common cancer, with around 3,100 new cases in 2017. About 850 women die of cervical cancer in the UK each year, averaging more than two deaths each day; mortality rates are highest among women aged 85-89 (2015-2017). Additional statistics:- Incidence rates in the UK are highest among patients aged 30-34 (2015-2017)
- Since the early 1990s, cervical cancer incidence rates have decreased by 25 percent in the UK, with these rates likely to fall in future decades, according to projections that account for the expected impact of HPV vaccinations
- An estimated 34,800 women who had previously been diagnosed with cervical cancer were alive in the UK at the end of 2010.