The unsung role of the radiation therapist in product development

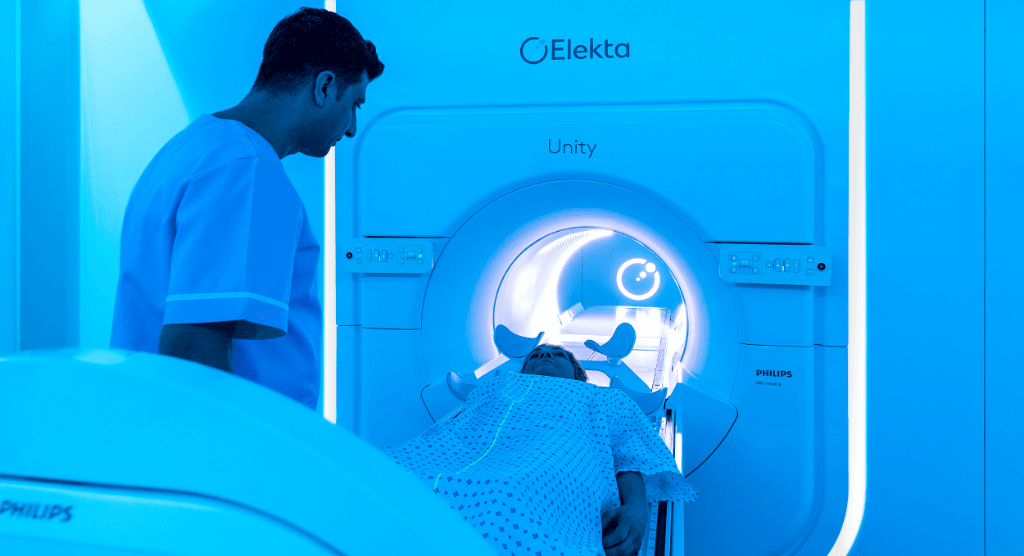
Elekta’s Liz Knowles reflects on her contributions in defining and refining IGRT, MRgRT workflows
According to licensed radiation therapist (RTT) and Elekta Unity product manager Liz Knowles, radiation therapy technology will fail if vendors don’t do four key things: involve the user upfront in development, take the time to develop and iterate on solutions carefully, push for consensus-driven standardization and design the technology for the mainstream user – not the experts.

Of the four, involving end users at the starting point is arguably the most critical. In the arena of radiation therapy, operating the treatment machine is the RTT’s domain. To ensure widespread adoption of Elekta’s IGRT (Elekta Synergy®) system and MR adaptive radiotherapy system (Elekta Unity), the input of radiation therapists was essential; new technology can’t simply be handed to clinical centers without having been tested by those whose sole job is to operate it efficiently and safely.
Knowles was at the ground floor of this testing for both Elekta Synergy and Elekta Unity. By 2003, Elekta had produced research prototypes of Elekta Synergy and had delivered them to institutions comprising the Elekta Synergy Research Consortium, which included Toronto’s Princess Margaret Hospital (PMH), among others.
“Between 2003 and 2006 I worked with PMH’s chief medical physicist,” Knowles says. “We field-tested the CBCT reconstruction, registration and workflow software in this novel integrated imaging workflow. With CBCT, RTTs had to learn new skills to be able to implement them in clinics. Before IGRT, we were really only looking at bony anatomy on 2D EPID images, but suddenly RTTs need to know exactly where the prostate, bladder and rectum are on 3D CBCT images.”
PMH hand-picked RTTs who demonstrated intense interest in the site’s research Synergy system and trained them how to recognize anatomical structures on CBCT.
“Elekta Synergy wasn’t something you could just chuck over the fence and expect it to be widely adopted and used.”
“Involving RTTs was key, because it was really important to implement something that could be operated by the average user,” she adds. “We needed to establish standardized imaging protocols that could be used out of the box, so the first clinical Synergy users didn’t have to spend time developing them. Elekta Synergy wasn’t something you could just chuck over the fence and expect it to be widely adopted and used.”
The workflow development phase entailed numerous dry runs, testing the imaging technology on phantoms and collecting imaging data during treatments of clinical trial patients for offline analysis only.
“We practiced the workflow extensively, mostly in the evenings when the treatment machine was not in clinical use, to just get as familiar as we could with the workflow, so that when we went live with that first patient everyone would be very comfortable with it,” Knowles says.
The work of PMH and the other consortium centers contributed tremendously to Elekta Synergy best practices and clinical applications as clinics around the world began acquiring the system.
On to Elekta for more Synergy work and MR-guided radiotherapy
By 2006, Knowles was “ready to give industry a try,” and she easily secured a position in the company. She continued her Synergy workflow refinement activities on subsequent releases (e.g., Symmetry 4D) for a couple of years, took two years of maternity leave, then returned in 2010 to help develop the Elekta Unity MR-Linac workflow.
How RTTs would navigate patient set-up, imaging, and plan adaptation on the MR-Linac were key workflow elements that needed careful consideration.
“Working with end users in the Elekta MR-Linac Consortium was brilliant – we could approach end users immediately and brainstorm with them in the room.”
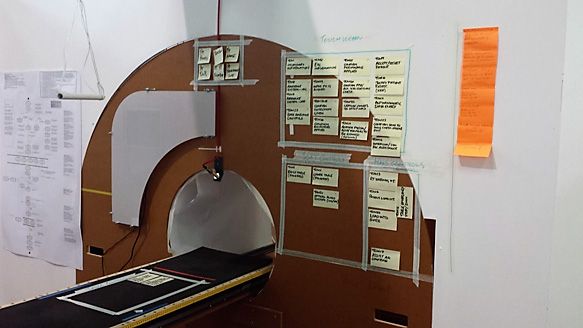
“We needed to map the workflows out,” she recalls. “Often it involved drawing the steps on large pieces of paper and testing them with end users – even without a prototype system to show them – asking them if our suggestions matched with how they envisioned the workflow. Or if there were superfluous steps that could be eliminated or tasks that could be parallelized rather than serialized. Working with end users in the Elekta MR-Linac Consortium was brilliant – we could approach end users immediately and brainstorm with them in the room.”
Sometimes, Knowles and her colleagues experienced push-back from RTTs, their stance on using lasers for setup, for example.
“We believed lasers were unnecessary and not having them would speed up the setup process and be more patient- and RTT-friendly,” she observes. “But sometimes, manufacturers need to be bold and drive a practice change. It wasn’t until users implemented the system clinically that they realized laser setup was redundant in the adaptive workflow. Evidence now shows that adapted plans are unaffected by wider setup tolerances.”
Conversely, the Elekta team embraced the wisdom of end user RTTs on other suggestions.
“We thought it would be good to project where patient positioning devices should be put on the table, versus just having a screen indicate which number to input,” Knowles says. “The users told us we were over-engineering a non-existent problem. Another of our ideas was to put a kiosk at the entrance to the maze where the patient would check in and do the MR eligibility check list, ID and biometrics. The users hated it, because it was forcing patients to stop physically at a fixed position, which froze the workflow.”
At times, Liz and her colleagues had RTTs engage directly with Elekta engineers, so the technical developers could identify with how RTTs navigated the workflow.
“You need engineers who can remain neutral and really listen to the feedback. Engineers can understandably get a bit defensive about ideas they’ve spent months working on.”
“You need engineers who can remain neutral and really listen to the feedback,” she says. “Engineers can understandably get a bit defensive about ideas they’ve spent months working on.”
Consortium RTTs were essential in sorting out the “human factors” side of the MR-Linac, evaluating the comfort/discomfort of a particular button when pushed continuously, for example, or a movement that required frequent bending over a table.
“We also obtained some insight on things like the wing board patient positioning device, which RTTs deemed uncomfortable and the first design even tipped,” Knowles recalls. “In addition, we realized that if you used the very last indexing point with the wing board and you lowered the table, the wing board clipped the bore. RTTs hated the first design of the hand grip, so we reiterated on that, and we took RTT input on the design of the anterior surface coil – we designed it so it wouldn’t touch the patient’s skin, but close enough to obtain maximum SNR.”
Over time, the workflow refinement evolved from sticky notes on a crude medium-density fiberboard (MDF) mockup of the MR-Linac to an actual bunker with real systems installed.
“The most intensive activity we did was to invite two RTTs from every consortium site, a total of 14 therapists, and a few physicists and oncologists,” she says. “We were trying to maximize input – letting these professionals share their opinions and use the system as they think they would use it, while at the same time structuring the feedback and making sure it didn’t become a big free-for-all.”
The assumption all along, according to Knowles, was that the MR-Linac workflow would have to align wherever possible to the traditional linac workflow.
“We knew that RTTs should be leading this workflow – it would be absolutely essential to get broader adoption of this technology.”

“We knew that RTTs should be leading this workflow – it would be absolutely essential to get broader adoption of this technology,” she says. “If a center’s radiation oncologist had to come to the treatment unit for every single patient treatment, we were sure staff at clinics would view that as just not feasible, not only from a financial standpoint, but also for practical reasons.”
Knowles’s work on Elekta Synergy and Elekta Unity demonstrates the dramatic evolution of the RTT’s potential role in product development as radiotherapy technology advanced.
“We went from lifting heavy Cerrobend blocks and patient positioning using skin marks alone to learning and implementing integrated imaging workflows and being the primary operators of the MR-Linac, the most advanced radiotherapy system ever developed,” she says. “For Elekta Synergy and the MR-Linac, RTTs were on the ground floor in influencing the design of the workflow, not only externally from Consortium RTTs invited to participate in the process, but also internally here at Elekta. It’s a career path that some RTTs may not have considered before.”