SmartClinic demonstrates potential to improve patient outcomes

New study demonstrates how MOSAIQ SmartClinic reduces the time from initial consult to treatment completion for head and neck cancer patients
The University of Mississippi Medical Center (UMMC) recently demonstrated that MOSAIQ® SmartClinic, in combination with other factors, such as accountability, motivation and leadership, significantly enhanced patient workflow efficiency and shortened the radiation therapy package time (RTPT) for head and neck cancer patients by an average of 22.9 days1.
Importance of package times
RTPT is the time from initial consultation to radiation therapy completion and forms part of the total package time (TPT)–the overall time from diagnosis to treatment completion–for cancer patients. TPTs can vary greatly, particularly for indications such as head and neck cancers that involve complex diagnosis and treatment processes across multiple disciplines. Reductions in TPT are highly desirable since evidence suggests that shorter TPTs often correlate to improved cancer patient outcomes for a variety of tumor sites2-10.
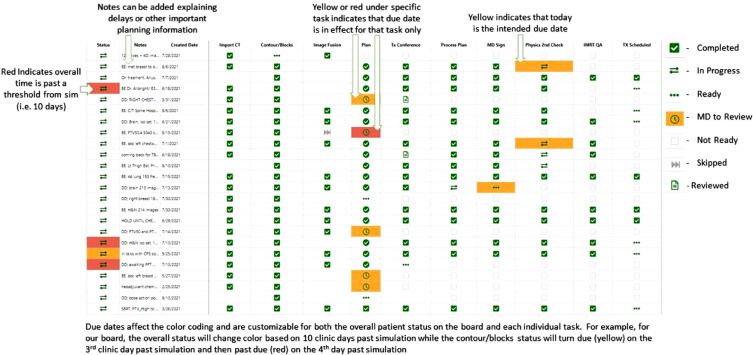
Recognizing this need for improved workflow efficiencies and package times for cancer patients, the team at UMMC implemented an automated patient management and accountability system – MOSAIQ SmartClinic with SmartBoard – to help visualize and track how well patients were hitting expected time points for each stage of their treatment workflow. Thanks to MOSAIQ and SmartClinic interoperability, the data input from MOSAIQ to the SmartBoard was automatic and seamless, and the SmartClinic displays could be easily customized to the needs of the department.
“Thanks to MOSAIQ and SmartClinic interoperability, the data input from MOSAIQ to the SmartBoard was automatic” and seamless.”
Replacing a paper-based tracking system, SmartBoard provided a visual display of patient workflows, which was reviewed most mornings in team huddles. The SmartBoard was always visible on a screen in the conference room and was accessible to any member of the team via any computer. In addition, to encourage accountability, a number of measures were introduced: the move to the new workflow was established as departmental policy; due dates for major workflow steps were assigned color-coded due dates; and open and host communication between project leads and staff was encouraged.
Measuring success
To measure the impact of SmartClinic on RTPT, the team compared critical time point data for head and neck cancer patients before and after SmartClinic implementation. Statistically significant mean reductions were observed for several steps in the patient workflow (table 1), resulting in a mean reduction of total RTPT of 22.9 days. Since the mean statistic alone is sensitive to outliers, median data was also reported, revealing a statistically significant and equally impressive median reduction in RTPT of 14 days. The authors describe this reduction in RTPT as “astonishing” and hypothesize that such package time improvement will translate into improved clinical outcomes. They acknowledge that evidence for this will require adding to their data set and ongoing follow up of patients.
“SmartClinic reduced RTPT by an average of 22.9 days.”
Table 1. Impact on treatment workflow steps following SmartClinic implementation
| Workflow step | Mean reduction (days) |
| Consult to first treatment | 13.4 |
| Simulation to first treatment | 4.2 |
| Simulation to treatment completion | 13.3 |
| First treatment to treatment completion | 9.0 |
| Total RTPT | 22.9 |
The new system has been received extremely well by oncology staff, with an intradepartmental survey revealing the following:
- An overwhelmingly positive impression of SmartClinic’s effect on individuals and the department.
- A relatively easy learning curve overall.
- Perceived increases in comfort, ability and teamwork.
One member of staff went as far as to say, “SmartClinic has been one of the single best things that has happened to our clinic.”
“SmartClinic has been one of the single best things that has happened to our clinic.”
Accountability and automation are key

The authors observed that the automation provided by SmartClinic was key to the success of this intervention, since previous attempts at a non-automated solution were unsuccessful. They were quick to point out that SmartClinic is a specific tool and, like any intervention, it requires ‘soft components’, such as accountability, motivation and leadership, to ensure that it is optimized and implemented in such a manner as to have the desired effect.
In fact, the authors commented that SmartClinic provided an opportunity to encourage healthy accountability through regular review of the SmartBoard together. This made it obvious when patients experienced delays and allowed the team to celebrate when all expected timepoints were achieved.
“SmartClinic provided an opportunity to encourage healthy accountability through regular review of the SmartBoard together.”
All of these factors combined to ensure dramatic improvements to head and neck cancer patient workflows at UMMC. The authors concluded that these positive results provide a compelling argument for patient workflow interventions and their future work will involve fostering collaboration with other departments to further reduce overall package time.
Find out how MOSAIQ SmartClinic can enhance efficiencies in your oncology department.
References
- Strategic Reduction of Package Time in Head and Neck Cancer. Adv. Radiat. Oncol. 2022 8(1): 101117. (Jan-Feb 2023) Duggar WN et al. https://doi.org/10.1016/j.adro.2022.101117.
- Assessment of time-to-treatment initiation and survival in a cohort of patients with common cancers. JAMA Netw Open. 2020;3: e2030072. Cone EB, Marchese M, Paciotti M, et al.
- Association of treatment delays with survival for patients with head and neck cancer: A systematic review. JAMA Otolaryngol Head Neck Surg. 2019;145:166-177.Graboyes EM, Kompelli AR, Neskey DM, et al.
- Defining optimal treatment times in head and neck cancer care: What are we waiting for? JAMA Otolaryngol Head Neck Surg. 2019;145:177-178. Houlton JJ.
- Impact of delays in radiotherapy of head and neck cancer on outcome. Radiat Oncol. 2020;15:202. Zumer B, Pohar Perme M, Jereb S, Strojan P.
- Impact of time to diagnosis and treatment in head and neck cancer: A systematic review. Otolaryngol Head Neck Surg. 2020;162:446-457. Schutte HW, Heutink F, Wellenstein DJ, et al.
- Impact of time factors on outcome in patients with head and neck cancer treated with definitive radio(chemo)therapy. In Vivo. 2017;31:949-955. Dahlke S, Steinmann D, Christiansen H, et al.
- The effect of treatment package time in head and neck cancer patients treated with adjuvant radiotherapy and concurrent systemic therapy. World J Otorhinolaryngol Head Neck Surg. 2019;5:160-167. Ghanem AI, Schymick M, Bachiri S, et al.
- The impact of radiation treatment time on survival in patients with head and neck cancer. Int J Radiat Oncol Biol Phys. 2016;96:967-975. Shaikh T, Handorf EA, Murphy CT, Mehra R, Ridge JA, Galloway TJ.
- Time abides long enough for those who make use of it. Cancers Head Neck 2018;3:11. Fareed MM, Galloway TJ.
LWBMQS230105





