Setting the PACE: The James Cook University Hospital boosts confidence in prostate radiotherapy

While prostate cancer is a serious condition, most men diagnosed in the early stages survive thanks to treatment options such as SBRT, in which there is increasing emphasis on hypofractionation with low treatment toxicity. For patients diagnosed with high-risk disease, researchers now want to determine whether additional targeting of the lymph nodes, alongside the prostate, can further reduce the risk of prostate cancer relapse.
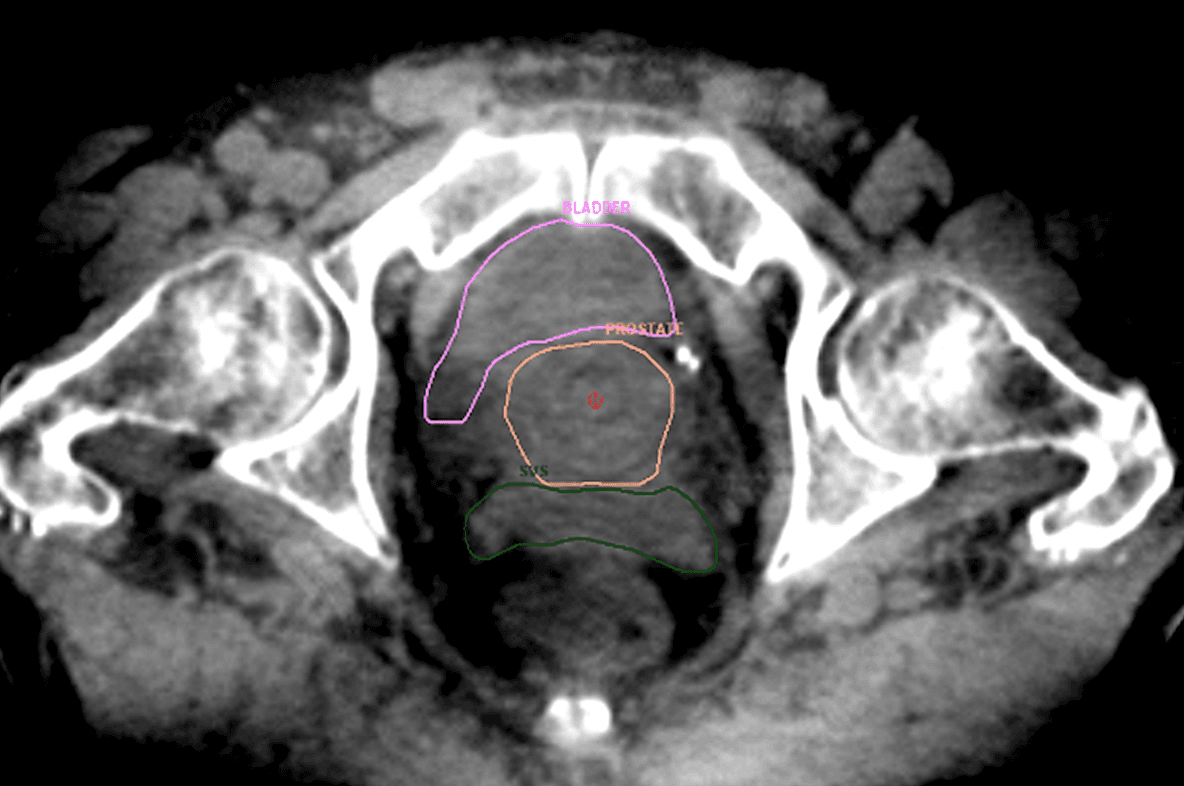
Clinicians at The James Cook University Hospital (Middlesbrough, England), have been key participants in the UK’S PACE (Prostate Advances in Comparative Evidence) trials since 2015, including the PACE-NODES trial, a phase III randomized study of five-fraction prostate SBRT versus five-fraction prostate and pelvic nodal SBRT. Doctors are able to visualize all relevant pelvic structures in prostate cancer radiotherapy with real-time imaging modalities from Elekta, while also monitoring the prostate’s position in real time to ensure that only the target receives radiation, while avoiding organs-at-risk.
The hypofractionated PACE-NODES prescription employed by the team at James Cook involves five VMAT fractions of 7.25 Gy for a total dose of 36.25 Gy. For treatment delivery, the hospital uses one of its six Versa HD™ systems, particularly utilizing Agility™ MLC and High Dose Rate mode (flattening filter-free [FFF]) for these higher dose treatments.
Elimination of intrafraction CBCT in PACE-NODES
In addition to being among the top UK patient recruiters for the PACE-A, PACE-B and PACE-C trials, James Cook is one of the first to open and recruit patients for PACE-NODES, since September 2022 enrolling nearly 40 patients. The center anticipates recruiting about four patients each month for the duration of the study to a total of over 100 patients.
Because of PACE-NODES’s high dose per fraction (7.25 Gy X 5), geometric misses caused by the prostate moving out of the target volume can be problematic.
“We need to know where we’re putting the dose,” RTT Andy Jepson notes. “With a typical 30-fraction or 20-fraction course, even if there are small geometric discrepancies day to day, they will smooth out over the complete course. However, in the absence of ultrasound technology to monitor prostate motion, with just five fractions the impact of prostate motion is higher.
“Therefore, for PACE-NODES participating institutions that don’t use real-time imaging, an intrafraction CBCT is a specific requirement of the trial if the treatment time exceeds three minutes,” he continues. “We’re continuously tracking prostate motion, so we don’t need to do a mid-fraction XVI. That saves the patient the extra dose.”
“We have confidence that we have delivered the dose to the right place.”
James Cook medical physicist Darren Thompson, PhD, adds: “We have confidence that we have delivered the dose to the right place. In our experience, most treatment fractions aren’t interrupted anyway, but it’s good to know that if movement does happen, the treatment will be safe.”
“For the PACE-NODES trial we use a real-time ultrasound-based soft tissue visualization solution and XVI almost exclusively for these patients,” says Dr. Thompson. “With SBRT’s longer treatment times there is more potential for prostate movement, and it is ideal for detecting that. Without real-time imaging we would be ‘blind’ for several minutes during beam delivery.”
According to James Cook radiographer Antony Pearson, RTT, James Cook is the only UK center to use XVI and ultrasound soft tissue visualization as complementary imaging modalities for prostate radiotherapy.
“Regarding XVI, although there is no practical substitute for intrafraction prostate monitoring, kilovoltage CBCT enables us to see structures that we’re unable visualize as well due to their distance from the ultrasound probe. These include the seminal vesicles and nodes, in addition to bladder filling and bowel position. That’s why we use this combined approach and do all our initial soft tissue matching using XVI.”
During treatment, the prostate position is continuously tracked; if it exceeds a five-millimeter threshold of movement in any of three axes (sup-in, left-right, ant-post) for five seconds the beam will be interrupted by the Elekta Response gating control interface.
“If the prostate were to move back into tolerance without intervention, the beam may be manually resumed,” he says. “If not, another CBCT is acquired, patient position corrected, monitoring resumed, and the beam restarted.”
The use of FFF (High Dose Rate mode) helps limit beam-on time for these treatments, whether with or without nodes.
“For prostate SBRT without nodes, beam-on time is 1.5 to two minutes, and for prostate with nodes [PACE-NODES], beam-on is three to five minutes, depending on plan complexity,” Dr. Thompson observes. “There are some very complicated shifts happening with prostate and nodes patients.”
A focus on patient comfort and dignity
A cancer diagnosis is stressful enough without the rigors, both minor and major, of disease treatment. James Cook caregivers appreciate their patients’ situation and strive to make prostate radiotherapy as anodyne as possible.
“Patient comfort is really important to us.”
“Patient comfort is really important to us,” Pearson says. “Our prostate patients must have a full bladder before treatment, but we try to have them not overfill to the point they’re uncomfortable, which could cause them to fidget and not lay still. We’re also aware that while we use a non-ionizing imaging tool, positioning the probe requires not insignificant pressure against the perineum with the patient’s legs bowed out. It’s not the least awkward posture to be in.”
Still, the staff’s concern about ensuring patient comfort and dignity led them to create a questionnaire/information document to assess patient opinion about their treatment.
“One hundred percent of patients surveyed agree that ‘the procedure was adequately explained to them prior to scanning,’” Dr. Thompson notes. “And that ‘The information was extremely/very helpful, and it was appropriate and clear to understand.’”
Dr. Thompson adds that more than 70 percent of patients always felt comfortable during the procedure, any lack of comfort attributable typically to the hard couch top rather than the equipment.
“Regarding probe positioning,” Jepson adds, “we always ask patients – both in surveys and in real time – if it feels OK when in place and we have found that this is tolerated really well. One of the questions aims to find out if patients felt ‘dignified’ during the procedure. Ninety percent of patients said they ‘always felt dignified.’”
As the future of radiotherapy is set toward increasing hypofractionation, the team at James Cook is setting the pace for this large and important patient cohort.
Learn more about Elekta’s radiation therapy solutions.
LAROX230803





