Pandemic puts focus on hypofractionated radiotherapy in Colombia

Patients with prostate or breast cancer receive shorter-course radiation therapy at Hospital San Ignacio
While many Colombian cancer patients experienced long delays in their radiotherapy treatment for prostate and breast cancer due to Covid-19 restrictions, the pandemic has encouraged and accelerated the adoption of hypofractionated protocols that have significantly shortened the patient’s cancer treatment journey.

“We started using hypofractionated radiotherapy – 60 Gy in 20 fractions – for our prostate cancer patients as early as April 2020,” says Juan Carlos Galvis Serrano, MD, lead radiation oncologist of the genitourinary malignancies multidisciplinary care team at Bogota’s Hospital San Ignacio, which treats about 80 prostate cancer patients each day. “Many patients preferred to defer treatment after the first Covid peak in August 2020 and many urologists put patients on hormonal block, which – compared with neoadjuvant hormonal block – has a better impact on metastasis, metastasis-free survival and overall survival, according to current evidence.”
In Colombia and South America, he adds, telemedicine is being implemented for follow-up visits, with active surveillance the preferred course for favorable intermediate-risk prostate cancer.
“Hypofractionation for prostate cancer represents a major change in the standard of care in radiotherapy.”
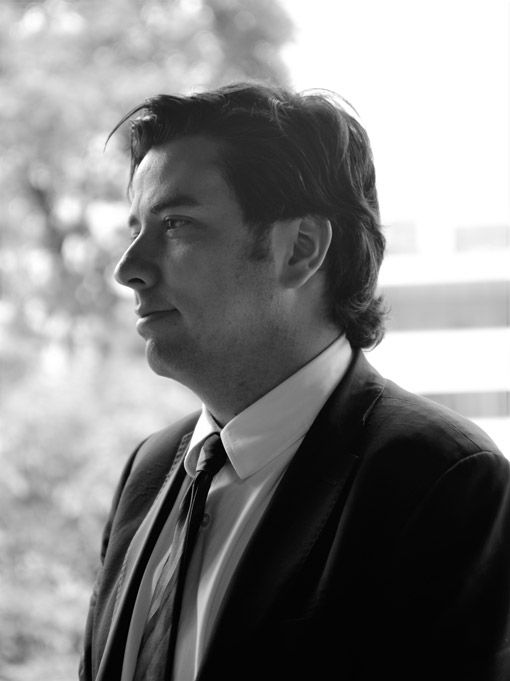
“In higher-risk disease, androgen deprivation therapy for deferred radiotherapy is considered safe for up to seven months,” he says. “Hypofractionation for prostate cancer represents a major change in the standard of care in radiotherapy with the most solid and robust evidence in the history of radiotherapy. It is supported by multiple phase III randomized, controlled trials.”1-7
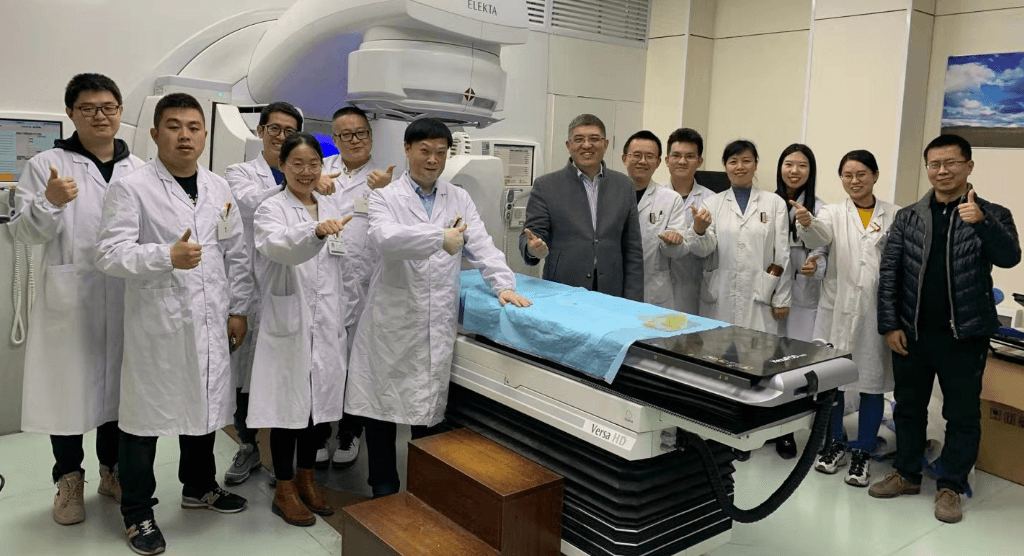
Hypofractionation has also benefited access among citizens of South American countries, which lack sufficient linear accelerators to accommodate their populations, Dr. Galvis Serrano says. He notes that the USA standard is one linac per 200 people, whereas in South America the ratio is one linac per one million inhabitants. Hospital San Ignacio operates three Elekta linacs.
“Whether it’s our breast cancer patients – who receive a 25 Gy treatment in just five sessions [80 patients each day] – or the 20-fraction prostate patients, shorter courses not only improve accessibility, they also put less strain on the patient’s finances due to work absences, which in turns helps boost a given country’s economy,” he observes.
In addition to the trend toward condensed radiotherapy courses, the pandemic also highlighted the importance of remote working arrangements facilitated by Citrix-based technology at Hospital San Ignacio. Dr. Galvis Serrano, himself, contracted asymptomatic Coronavirus in March 2020, which had him quarantined for 20 days.
“The radiotherapy service decided to purchase the remote access license, because the staff health and ability to work on-site would always be a question during 2020 and beyond,” he says.
“I wasn’t able to take advantage of remote working during my quarantine, but after that period I and the other radiotherapy staff could take advantage of the technology to limit their exposure to the virus in the hospital. I think because of the pandemic, telemedicine will continue to improve, using virtual boards and remote target volume delineation capabilities for treatment planning and plan approvals.”
Learn more about Elekta linacs.
References
- Morgan SC, Hoffman K, Loblaw DA, et al. Hypofractionated radiation therapy for localized prostate cancer: An ASTRO, ASCO, and AUA evidence-based guideline. Journal of Clinical Oncology 2018 36:34, 3411–3430.
- Dearnaley D, Syndikus I, Mossop H, et al. Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. 2016 Aug;17(8):1047-1060. doi: 10.1016/S1470-2045(16)30102-4. Epub 2016 Jun 20. Erratum in: Lancet Oncol. 2016 Aug;17 (8):e321. PMID: 27339115; PMCID: PMC4961874.
- Lee WR, Dignam JJ, Amin M, et al. NRG Oncology RTOG 0415: A randomized phase III non-inferiority study comparing two fractionation schedules in patients with low-risk prostate cancer. Journal of Clinical Oncology 2016 34:2_suppl, 1-1.
- Incrocci L, Wortel RC, Alemayehu WG, et al. Hypofractionated versus conventionally fractionated radiotherapy for patients with localised prostate cancer (HYPRO): final efficacy results from a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2016 Aug;17(8):1061–1069. doi: 10.1016/S1470–2045(16)30070–5. Epub 2016 Jun 20. PMID: 27339116.
- Brand DH, Tree AC, Ostler P, et al. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. Lancet Oncol. 2019 Nov;20(11):1531–1543. doi: 10.1016/S1470–2045(19)30569-8. Epub 2019 Sep 17. PMID: 31540791; PMCID: PMC6838670.
- Dunlop A, Mitchell A, Tree A, et al. Daily adaptive radiotherapy for patients with prostate cancer using a high field MR-linac: Initial clinical experiences and assessment of delivered doses compared to a C-arm linac. Clin Transl Radiat Oncol. 2020;23:35-42. Published 2020 Apr 29. doi:10.1016/j.ctro.2020.04.011
- https://clinicaltrials.gov/ct2/show/NCT03367702