Optimizing needle insertion with CT guidance during GYN brachytherapy

Study at Turkey’s Liv Hospital Ulus reports that CT in the intracavitary/interstitial brachytherapy workflow is feasible and increases safety and efficiency
Using CT to guide and plan intracavitary/interstitial brachytherapy for patients with cervical cancer is an attractive option for centers with limited 3D imaging options for determining needle use and location, a recent study asserts.1

Whether done with or without image guidance, it is reported that adding needles to intracavitary brachytherapy significantly increased the three-year local control rate by 10 percent, without substantially increasing toxicity in patients with locally advanced cervical cancer.2 It not only permits adequate-dose coverage of the parametrial tumor extension, but it also overcomes suboptimal applicator positioning issues.2
According to CT study co-author Merdan Fayda, MD, radiation oncologist at Liv Hospital Ulus (Istanbul, Turkey), the use of CT scans after applicator insertion (CT preneedle) and following needle placement (CT postneedle) is a practical method for deciding whether to perform intracavitary/interstitial brachytherapy and informs optimal needle placement. CT guidance also results in fewer unloaded needle insertions or complications, and higher dose contribution of needles that are inserted and loaded (i.e., dwell intensity).
“There are no international guidelines for optimal needle insertion during intracavitary/interstitial brachytherapy for cervical cancer.”
“There are no international guidelines for optimal needle insertion during intracavitary/interstitial brachytherapy for cervical cancer,” Dr. Fayda says. “Although an MRI scan is performed in the last week of EBRT to evaluate the indication for intracavitary/interstitial brachytherapy, post-EBRT MRI can’t assess organ movement and suboptimal applicator insertion that could influence the channels in which needles are inserted, and there are no data on how needles may be shifting after insertion.”
The study aimed to explore the clinical feasibility of CT-guided needle use and to assess differences between the planned and inserted needles in terms of shift magnitude.1
CT-guided needle insertion
To reinforce the decision to add interstitial needles in the brachytherapy treatment – based on the post-EBRT MRI scan – the researchers performed two CT scans (preneedle and postneedle) for each of the patients’ four fractions.

“For our 24 patients at Liv Hospital Ulus, we inserted the tandem-and-ovoid applicator in the OR, then the patients were brought to the CT room for the CT preneedle scan,” Dr. Fayda explains. “We took about five minutes to review this scan to determine the needle channels and insertion lengths, and to assess the applicator position, OAR proximity to the target, and the parts of the target that extended past the applicator’s coverage capacity.”
Based on this evaluation, if clinicians determined that needles weren’t required for a given fraction, the patient would receive intracavitary brachytherapy only, which was planned with the CT preneedle scan. If the CT preneedle scan confirmed that patients could benefit from intracavitary/interstitial brachytherapy for a given fraction, needles were inserted in designated channels with the patient on the CT table. Three-dimensional brachytherapy planning was performed on the center’s Oncentra® Brachy planning system after contouring the GTV, CTVHR, and OAR (bladder, rectum, sigmoid, small bowel) on the CT postneedle scan.
The entire CT preneedle, needle insertion and CT postneedle process took up to 20 minutes, depending on the number of needles inserted.
A total of 266 interstitial needles were inserted under CT guidance among the 24 patients, encompassing 76 of 93 brachytherapy fractions. For 17 patients, needle insertion was avoided in one or more of the treatment’s four fractions.
Nominal needle shifting
The study also sought to qualify and quantify how needles are straying from their predetermined path once inserted, something that has been unclear for many practitioners of intracavitary/interstitial brachytherapy, particularly those new to the modality, Dr. Fayda observes.
“Before our study, it was unknown how the needles are traveling through the paracervical area, so we examined our needles’ pathway by using the needle-channel axis to determine the positional differences between the planned and inserted needles,” he says. “The difference between CT preneedle and CT postneedle was just 2.0 millimeters plus or minus 2.3 millimeters, with the shift occurring mainly in the posterolateral and posteromedial directions.”
Dr. Fayda adds that the shift magnitude was greater in needles with longer insertion lengths, but that none of the shifts required needle position adjustment (i.e., reinsertion) or repeated CT scanning in any of the patients.
Fewer unloaded needles
Because each patient had a CT preneedle scan for each fraction, there was greater certainty that any needles inserted were loaded. According to the literature, inserted unloaded needles can increase the risk of complications, such as hematuria, perineal infections and vaginal bleeding, Dr. Fayda notes.
“In this study, the frequency of inserted, unloaded needles was four percent – just 11 out of 266 needles.”

“One study of intracavitary/interstitial brachytherapy found that one of every five [20%] needles inserted was not loaded after insertion,” he notes. “We even observed this issue at our own institution among patients treated within the first three months after we implemented intracavitary/interstitial brachytherapy, but this most likely reflects our learning curve. However, in this study, the frequency of inserted, unloaded needles was four percent – just 11 out of 266 needles.”
Liv Hospital Ulus researchers also evaluated the dwell intensity of all needles within a fraction (i.e., summed dwell time of all needles inserted in a fraction as a percentage of total dwell time in the fraction). Again, the ability to use the CT preneedle scan enabled clinicians to boost the efficiency of needle use.
“A study in the literature reported 22 percent, whereas our study achieved 37 percent,” he says. “In addition, the average dwell intensity of individual needles was also higher at 11 percent versus the seven percent reported in another study. The combination of fewer unloaded needles and higher dwell intensities shows that repeated CT guidance increases the overall efficiency of interstitial brachytherapy.”
MRI versus CT
Although MRI’s superior visualization of OAR and tumor boundaries has seen increasing numbers of centers using the modality for brachytherapy planning, Dr. Fayda points out that his center’s use of CT-guided planning of intracavitary/interstitial brachytherapy has advantages.

“In all of our cases, the patient still has an MRI scan before and after EBRT – and we also want to use our new Elekta Unity MR-Linac for brachytherapy planning,” he says. “However, we prefer our method of CT-guided planning for several reasons. These include better reconstruction of the applicator and inserted needles and the fact that doing MRI preneedle and postneedle would be too time-consuming and labor intensive and require an MR-compatible obturator needle. Plus, with MR-guidance, the time before treatment application would be too long, which could potentially cause a shift in the applicator, thus negating the reliability of the preneedle scan.”
Liv Hospital Ulus uses a conventional 64-slice CT scanner for its methodology, which requires patients to be transferred from the CT room to the operating room for scanning and applicator/needle insertion, respectively. However, Dr. Fayda envisions a best-case-scenario with the new Elekta Studio, featuring the ImagingRing mobile CT scanner.
“Having Elekta Studio is my dream. Logistically, it would be best to have the imaging system in the brachytherapy OR, where we could image, plan, adapt and treat the patient in a single, dedicated room.”
“Having Elekta Studio is my dream,” he says. “Logistically, it would be best to have the imaging system in the brachytherapy OR, where we could image, plan, adapt and treat the patient in a single, dedicated room. With the ImagingRing, we could acquire in-room 3D imaging at the time of treatment. We have used a surgical C-arm for 2D imaging for transperineal insertions, but the ImagingRing could provide both 2D and 3D views of insertions for these cases. In addition, for prostate HDR brachytherapy cases, it would be very reasonable to fuse MRI images with real-time CT with patients treated in the high lithotomy position.”
CT-guided now routine
Having demonstrated the feasibility of CT-guided intracavitary/interstitial brachytherapy for cervical cancer, Liv Hospital Ulus clinicians use the methodology routinely for the approximately 20 cervical cancer patients each year who require brachytherapy boost.
“The rationale for the study was our desire to share this safer technique of inserting needles in the paracervical area, providing an effective dose to the CTVHR, while also sparing the rectum, bladder and sigmoid from excess dose,” he says. “At least one-third of these cervical cancer cases may need paracervical needle application. Hopefully, brachytherapists that are reluctant to implement intracavitary/interstitial brachytherapy due to uncertainty in needle insertion, or centers that don’t have MRI, will be encouraged to try this CT methodology.”
Learn more about Elekta’s brachytherapy solutions.
Dr. Fayda on GYN applicators
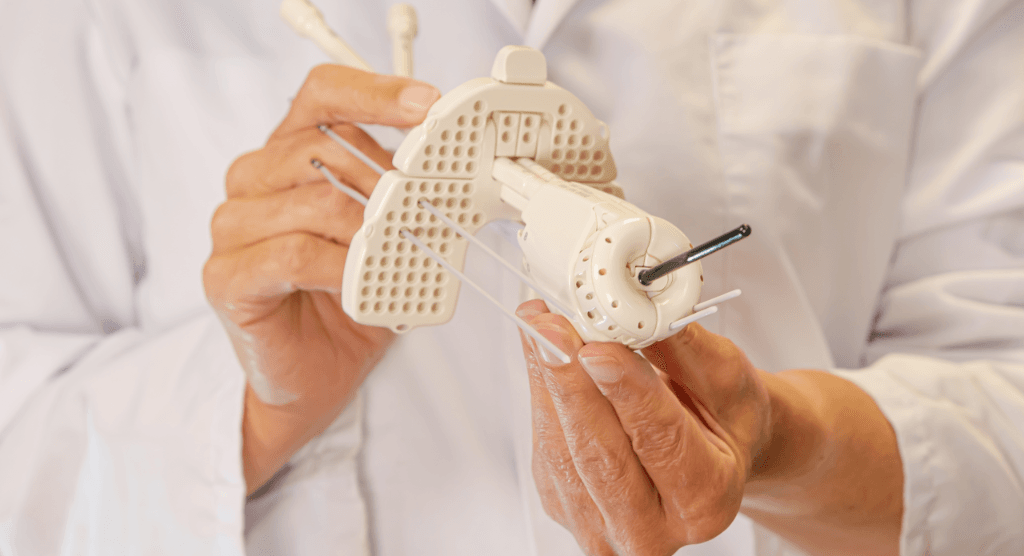
Although the Practical Radiation Oncology study that Liv Hospital Ulus researchers conducted employed Elekta’s discontinued Utrecht applicator, the center uses Elekta’s Venezia™ Advanced Gynecological Applicator clinically now and plans to acquire the company’s Geneva Universal Gynecological Applicator in the near future.
“The best thing about Venezia is its flexibility and ease of implementation, with the two semilunar ovoids that mimic a ring applicator,” Dr. Fayda says. “The two different tandem angles help in individualizing treatment. The semilunar ovoids can be perfectly located on the tandem after it is placed. Immobilization is also very easy. And the oblique needles are fantastic for covering lateral tumor extensions that go far beyond the conventional applicator range.
“In addition, in my view, Geneva is an improved version of the Utrecht applicator and we will have it very soon,” he adds. “Both the Geneva and Utrecht applicators can cover difficult anatomy, such as a retroverted or lateralized uterus, closed cervical channel and vaginal cuff relapses far beyond the vagina.”
References
- Tambas M, Tavli B, Bilici N, Dizman A, Sertel H, Fayda M. Computed tomography-guided optimization of needle insertion for combined intracavitary/interstitial brachytherapy with Utrecht applicator in locally advanced cervical cancer. Pract Radiat Oncol. 2021 Feb 5:S1879-8500(21)00043-6. doi: 10.1016/j.prro.2021.01.008. Epub ahead of print. PMID: 33556579. https://doi.org/10.1016/j.prro.2021.01.008.
- Kirisits C, Lang S, Dimopoulos J, Berger D, et. al. The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: Design, application, treatment planning, and dosimetric results. International Journal of Radiation Oncology*Biology*Physics, Volume 65, Issue 2, 2006, pages 624-630, ISSN 0360-3016, https://doi.org/10.1016/j.ijrobp.2006.01.036.