Korean medical center marks one-year anniversary with country’s first Elekta Unity MR-Linac

Gangnam Severance Hospital’s patients benefit with MR-guided radiotherapy’s enhanced target/OAR visualization, especially for breast, prostate and liver cancers
The imperative for Gangnam Severance Hospital’s (Seoul, Korea) radiotherapy department to continue improving its treatment capabilities drove the center’s radiation oncologists in 2019 to begin exploring their options. Officials concluded that MR-guided radiation therapy with the Elekta Unity MR-Linac would be an excellent addition to its equipment array, which includes an Elekta Versa HD® linac.

“You always consider something new and innovative in a treatment system, something that will help us treat patients better,” says Jun Won Kim, MD, PhD, Head of Radiation Oncology at Gangnam Severance Hospital. “One of our goals in selecting an MR-Linac was to introduce the most advanced radiation treatment system available and provide patients with the best cancer management. Plus, there is growing momentum for MR-guided radiotherapy and an appreciation of its benefits in the radiotherapy community.”
In procuring an MR-Linac, the hospital had two alternatives – the 1.5T Elekta Unity and another vendor’s 0.35T system.
“The 1.5T field strength provides much better image quality, and the Philips MRI integrated in Unity is proven technology.”
“The image quality difference between 0.35T and 1.5T is significant,” he says. “The 1.5T field strength provides much better image quality, and the Philips MRI integrated in Unity is proven technology. Although at the time the 0.35T system had the advantage of gating, it could only show motion monitoring MRI in a single plane. Unity is capable of showing MR motion in three planes, so when Unity introduces gating that would give us an advantage.”

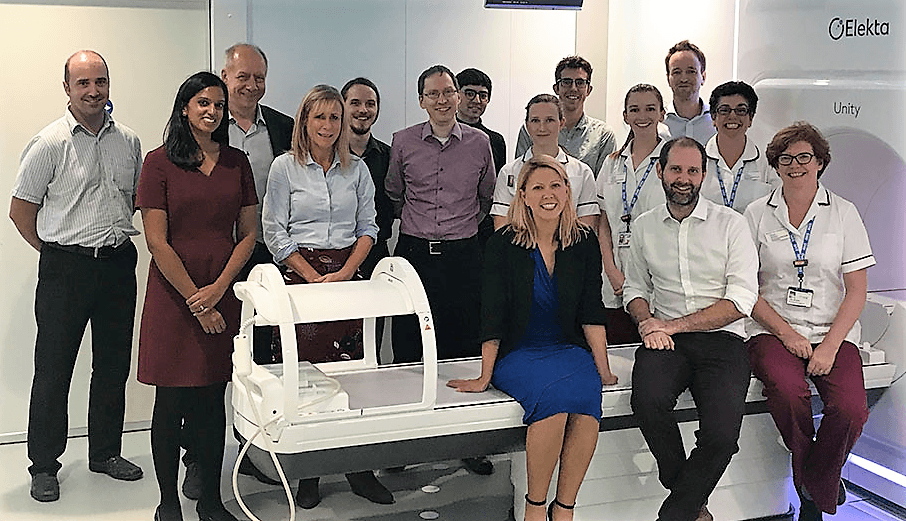
Under the direction of then-department chair Prof. Ik Jae Lee, and with the help of Elekta Korea in negotiating the price and financing of Elekta Unity, Gangnam Severance Hospital acquired the MR-Linac in 2021. Clinicians began treating their first patient, a prostate cancer case, on August 23, 2021. Throughout the following year, Severance Hospital physicians have benefited from the efficiency and real-time visualization of the Elekta Unity MR-Linac.
Online efficiency for prostate cases and more
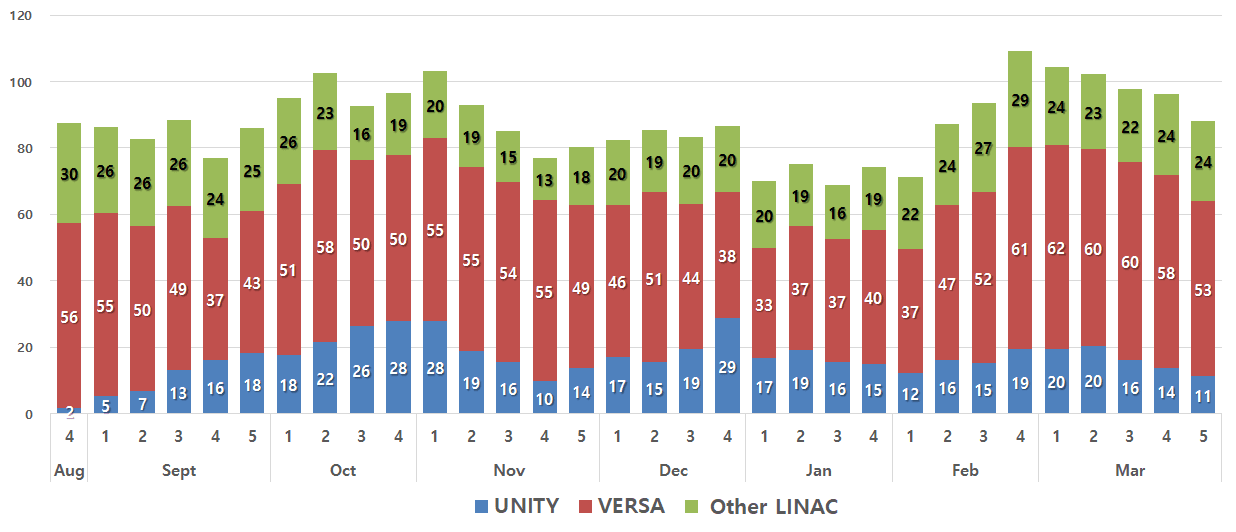
Severance hospital has sustained a commendable throughput of between 15 and 25 patient treatments each day on Elekta Unity; since clinical go-live, the system has been used for more than 390 patients during the first year of operation. (Figure 1) The ability to adapt radiation therapy online has been the key to the system’s efficiency.
“Unity is a productive system because it provides online adaptive radiotherapy.”
“Unity is a productive system because it provides online adaptive radiotherapy,” Prof. Kim notes. “Offline MR guidance would require us to take patients off the treatment table for rescanning with CT simulation followed by replanning. Therefore, patients must wait two or three days to continue treatment. So, beyond the image quality benefits of Unity, real-time motion monitoring has been a huge efficiency advantage.”
For example, for Severance Hospital’s prostate cases, which represent about 30 percent of the total Elekta Unity treatments for cancer, online adaptive radiotherapy is a critical time-saver.
“In daily prostate treatments, the environment changes with bladder filling and whether there is stool or gas in the rectum, which can change the prostate’s position and dose to these organs-at-risk,” he says. “If offline image guidance is used, the target and surrounding organs-at-risk are invariably in different positions. With online motion monitoring, we can track in real time the prostate’s position and its location relative to surrounding structures, which eliminates the need to replan in most cases.” (Figure 2)

Figure 2. Motion monitoring MRI can detect the position of the target and organs-at-risk in real time. Captured here is a rare instance of flatulence during treatment.
The first Elekta Unity case at Severance Hospital (August 23, 2021), was definitive radiotherapy for prostate cancer and involved a 2.5 Gy X 28 dose/fractionation schedule.
On October 7, the department switched to the 60 Gy X 20-fraction PRISM protocol for the first time, delivering 3.0 Gy X 20 fractions to the prostate and 2.2 Gy X 20 fractions to the pelvic lymph nodes.
“Before Unity, we had been using rectal ballooning for treating prostate cancer with the megavoltage system to reduce daily setup error and rectal toxicity,” Prof. Kim explains. “However, with the Unity system’s MR-guidance and online adaptive planning capability, we no longer felt the need to use rectal ballooning, and we decided to adopt the PRISM hypofractionated schedule to improve the patient’s compliance and quality of life.”
In addition to using Unity to treat prostate cancer patients, the hospital harnesses their system to treat liver tumors (~ 30 percent), breast cancer (~ 30 percent), in addition to lymph node metastases, rectal cancer and primary lesions at other sites.
Treating the mobile liver
Half of Gangnam Severance Hospital’s liver cancer cases are for primary hepatocellular carcinoma (HCC), an indication with a high incidence in Korea, in addition to single or multiple liver metastases.
Perhaps even more so than the prostate, in Prof. Kim’s view, the liver is subject to displacement from diaphragm motion – sometimes as much as five centimeters – when the tumor is in the dome of the liver. Radiation oncologists use respiratory control and abdominal compression in these cases and also rely on the Unity system’s real-time motion monitoring. Location of the bowel and stomach is critical in delivering radiation to the target within the liver.
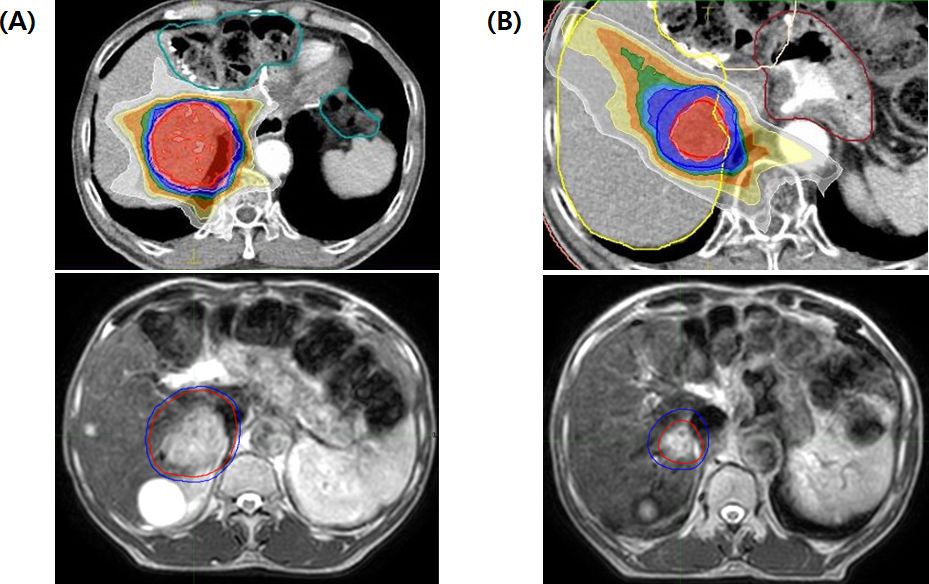
“The intra- and interfractional variation is a huge issue in liver treatments,” he says. “However, by virtue of better visualization of soft tissues with MR compared to MVCT or CBCT, you can see the target and the liver contour and vessels quite well. I feel more confident treating these patients with Unity and it’s my first choice for liver cases". (Figure 3)
Boosting the breast
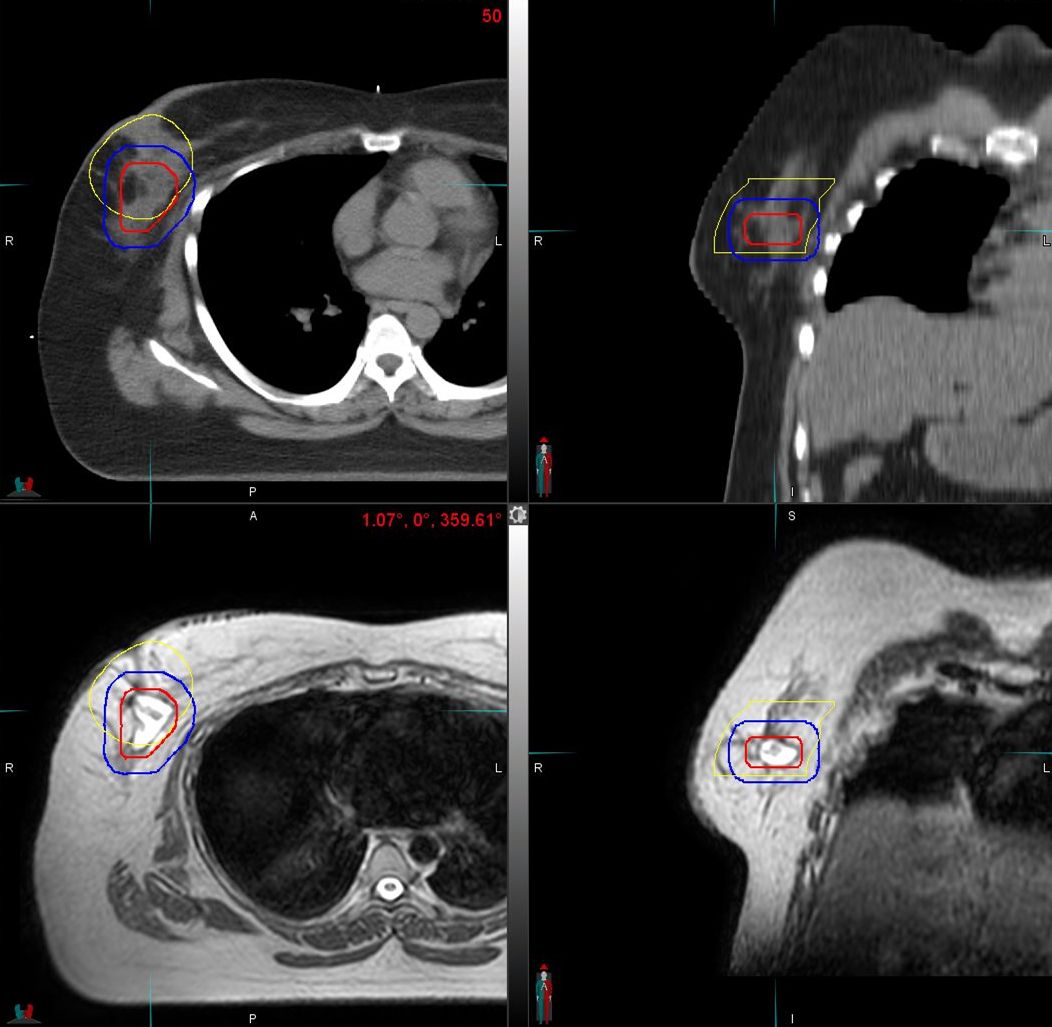
In breast cancer cases, the ability of Unity to visualize the post-operative surgical bed has made the MR-Linac indispensable.
“We use Unity to deliver a boost dose to the surgical bed after whole breast irradiation,” he says. “With the MR-Linac the margins of the surgical bed are more clearly depicted compared to CT.” (Figure 4)
Precision for difficult cases
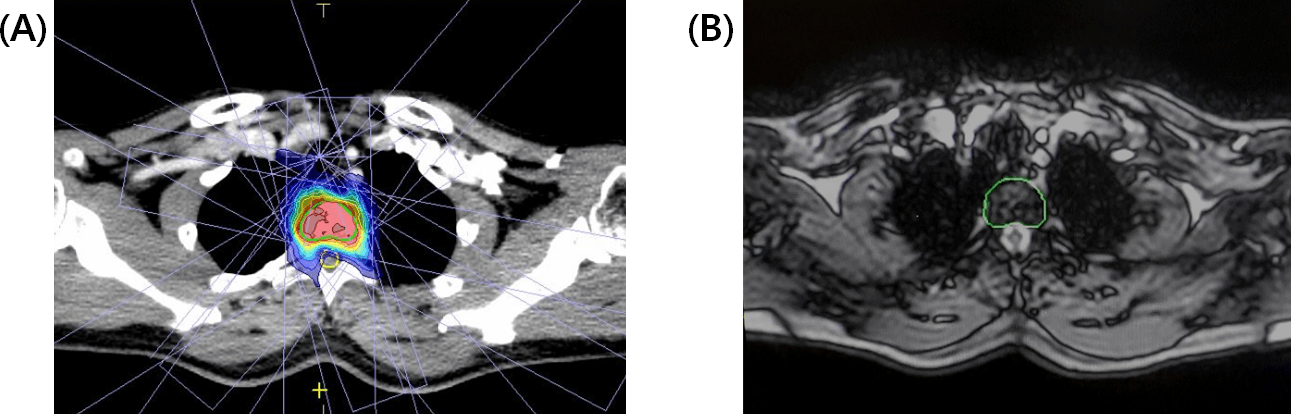
Although breast, prostate and liver cases comprise about 90 percent of Unity cases, some cancers present challenges that require exceptional visualization of sensitive structures.
“If I see a bone metastasis close to the spinal cord or other critical organs, I will choose the MR-Linac if the patient can accept the treatment time,” Prof. Kim observes. “MRI can clearly resolve the spinal canal and spinal cord (Figure 5). Without that degree of visualization, we’re uncomfortable prescribing a high dose, especially when we treat with SBRT. However, with Elekta Unity I’m confident that I will not deliver an excessive dose to the spinal cord.”
Streamlining the Elekta Unity MR-Linac workflow
During the past year, radiation oncology department staff have been working to streamline the Elekta Unity workflow, which – owing to the extra patient setup, imaging, data transfer and other steps – is longer than that of the traditional linac workflow.
“Depending on whether its Adapt to Position [ATP] or Adapt to Shape [ATS] daily plan adaptation [see “ATP/ATS plan adaptation”], with prostate – if there’s no recontouring as in ATP – treatment will be 30 to 35 minutes,” he says. “But when you have to recontour, as in ATS, the treatment time could go up to 40 minutes or longer. And if there’s ATS with hypofractionation or SBRT the treatment time could be 60 minutes.”
To ease the burden on the radiation oncologists, the department assigned recontouring of organs-at-risk in ATP plan adaptation to the radiation therapists.
“From the beginning we also have been using a video capture system for online treatment monitoring,” Prof. Kim adds. “Essentially, it’s a way to monitor the treatment remotely when a senior resident or fellow is called upon to recontour in the absence of the attending physicians – for example, if I’m seeing patients or away at a conference. It makes it more efficient for the RO to review.”
Patients have a role in making the Unity workflow more efficient as well, he adds. In cases that call for respiratory control, staff train patients on shallow breathing techniques and encourage them to practice at home.
“During treatment it makes their breathing more regular and reduces excess motion that could compel us to interrupt the therapy,” Prof. Kim explains.
In prostate cases, bladder filling is the principal issue.
“We emphasize bladder filling about two hours before treatment – so the bladder is not full, but it is sufficiently full to treat appropriately, ” he says. “In the beginning of the training the patients feel it’s difficult, but after the first few fractions they become more comfortable with it. That helps reduce rescanning and recontouring.”
Upcoming indications, MRgRT research and future aspirations
Beginning their second year of Unity use, Gangnam Severance Hospital clinicians are anticipating adding more treatment sites (e.g., brain cases) and initiating more Unity-related activities. For example, Elekta Unity has strengthened the radiation oncology department’s research potential.
“The MR-Linac allows the accumulation of high-resolution daily MR images during treatment,” Prof. Kim says. “Currently, ongoing studies include prostate, HCC and breast cancer trials. Combining high-quality MRI data and artificial intelligence models enables MRI-based auto-segmentation and radiomics studies. To this end, we are developing a centralized data storage system for collecting simulation CT and image-guidance CT/MR data.”
Radiotherapy customized for each patient
In Prof. Kim’s view, Elekta Unity provides truly individualized radiotherapy treatment for the first time by virtue of online adaptive radiotherapy and high quality images.
“In conventional RT planning you have one plan that you carry throughout all fractions, or you could spend the time to perform offline adaptive treatment,” he says. “With Unity, every fraction can be individualized according to the patient’s body changes, tumor changes and OAR changes. You can adapt daily to those variations.
“So far, Unity has met our expectations,” Prof. Kim adds. “The system has given Gangnam Severance Hospital a competitive edge, as we are surrounded by three of Korea’s largest hospitals, one of which has a proton therapy program. While Gangnam Severance Hospital is smaller in size, we have strong oncology programs, and we expect that Unity will continue to improve patient-specific, individualized cancer management at our hospital.”
Learn more about Elekta Unity MR-Linac.
ATP/ATS plan adaptation
MR-guided radiotherapy with Elekta Unity MR-Linac enables two different types of daily plan adaptation: Adapt to Position (ATP) and Adapt to Shape (ATS), both of which permit changes to the therapy that compensate for shifts in target position or treatment-related changes in target shape for each patient. In ATP, the shape and weight of beam segments in the reference plan are adjusted to match the current position of targets and organs-at-risk (OAR) based on rigid registration. In ATS, a new plan is created to match the anatomy of the day using deformable registration for contour propagation from the reference plan to the session MRI, followed by manual adjustment of the contours if necessary.