Improving cancer care in rural America

Doctors at two GenesisCare centers share their insights on the challenges and opportunities in serving patients in more remote areas
Patients who face difficulties in receiving appropriate cancer care typically live in developing countries, such as India and those in sub-Saharan Africa, but in reality, the challenge of cancer care access can occur anywhere in areas outside of major metropolitan centers. Despite the undisputed world-class cancer treatment services provided in the United States, individuals in thousands of US rural communities face a wide range of problems, as described in a recent JCO Oncology Practice article1. The authors cite how long travel distances and the length of a treatment course can be hardships for rural patients. This is a particularly grave issue, as well, since cancer-related mortality and other negative treatment outcomes are statistically higher in these regions. Clinicians at two GenesisCare centers, Foster Lasley, MD, in Oklahoma and Daniel Baseman, MD, in North Carolina, discuss how their respective centers are serving the cancer care needs of their rural patients.
Raising the bar in Oklahoma
With the seventh highest cancer mortality rate (per 100,000) among all states, Oklahoma’s cancer statistics2 are grim:
- 38 percent of the state’s population lives in federally designated rural counties. This percentage is more than 2.5 times the national average of 14 percent.
- Oklahoma’s rural residents of all races experience an overall cancer incidence that is 5.8 percent higher than the United States (all races) rate. However, they have an overall cancer mortality rate that is 15.5 percent higher than the corresponding US rate.
- Compared to the US (all races) rate, incidence rates for Oklahoma’s rural residents of all races are more than 20 percent higher for lung and cervical cancer, and mortality rates are more than 20 percent for lung, colorectal, kidney and cervical cancer.
Radiation oncologist Foster Lasley, MD, began working at GenesisCare’s Muskogee, Oklahoma and Rogers, Arkansas cancer clinics in August 2020, just three months after the company acquired the facility from another group practice.

“When I first started covering the Muskogee center we had an old Varian 2100, which didn’t have the ability to deliver stereotactic treatments, so we had to send them to a Tulsa clinic,” he says. “Also, DIBH for breast cancer patients was out of the question; the previous radiation oncologist had been using older techniques and standard long-course fractionation.”
Dr. Lasley knew that standard fractionation schemes for most indications presented a burden for cancer patients in northeast Oklahoma; the poverty rate is relatively high – owing to a 52.8 percent labor participation rate in Muskogee itself – travel distances are long for many in this part of the state and fuel was getting increasingly costly. Consequently, on his arrival to the Muskogee clinic he began hypofractionating treatments.
“This has really helped my breast cancer patients,” he notes. “The dated way to treat these patients is 32 fractions, but I can get it done in 20 fractions, including the boost, meaning they don’t have to spend the time and money to travel to the clinic. As a bonus, the patients are experiencing fewer side effects.”
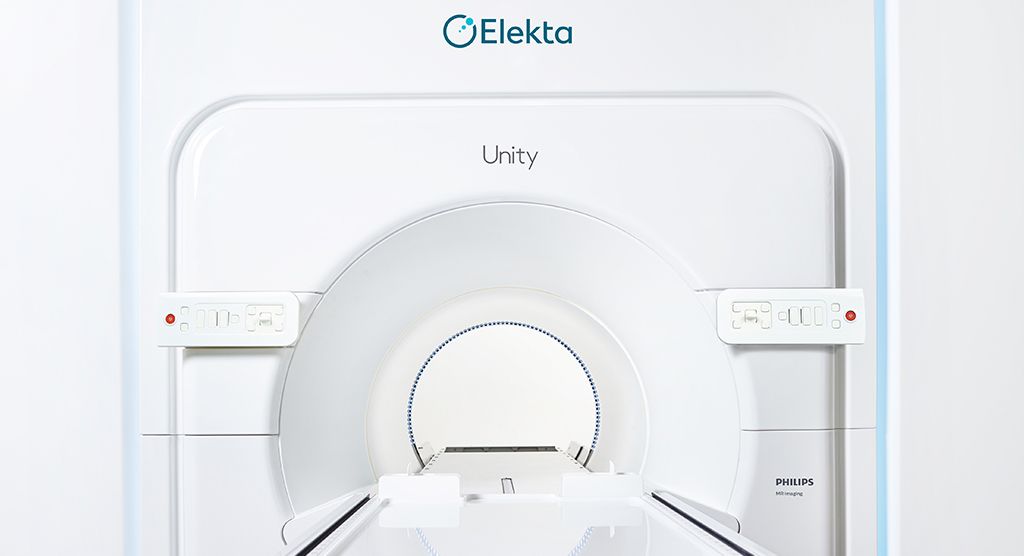
Recognizing that the Muskogee clinic’s technological capabilities could be improved, GenesisCare purchased a Versa HD™ linac for the center, as well as the Vision RT surface guided radiation therapy system, both of which became operational in March 2021.
“With this equipment I have been able to deliver DIBH for left-sided breast cancer patients – for maximum heart sparing – as well as SBRT, VMAT and motion control for other indications, such as prostate cancer. With SBRT, I can use a five-fraction schedule for intermediate- and low-risk patients. I lean even heavier that way if they’re coming from really far away. And, for high-risk prostate patients who come from far away and resist the idea of 44 fractions, I can hypofractionate down to 20 fractions.”

The ability to deliver SBRT also has benefited Muskogee lung cancer patients.
“When I first arrived here, we had a patient under a 35-fraction treatment for a tiny lung tumor – this was a protocol started by my predecessor,” Dr. Lasley recalls. “That’s just not nice to the patient. Now, with SBRT, I almost always treat patients like this with three to five fractions.”
A recent GenesisCare innovation that relies on Versa HD VMAT capabilities is establishment of a Skinviva™ program at the Muskogee site. Skinviva is widefield arc therapy over a broad skin area that encompasses not only known cancer, but also pre-cancerous lesions to prevent them from progressing into skin cancers.
“This therapy would not have been remotely possible with our previous linac, because it requires VMAT arcs for the broad, but shallow dose distribution over curved surfaces,” he observes.
In a single year, the GenesisCare Muskogee facility has made great progress in improving access to radiotherapy and convenience for its rural patients, via a combination of increased hypofractionation since Dr. Lasley’s entrance, in addition to the acquisition of its state-of-the-art Versa HD linac.
“Sophisticated techniques and technology have really closed the gap between what a rural center can do and what patients receive in metropolitan places…”
“Sophisticated techniques and technology have really closed the gap between what a rural center can do and what patients receive in metropolitan places like Tulsa,” Dr. Lasley says.
Distributed network of RT clinics benefits rural North Carolinians
While the western third of North Carolina is blessed with the natural beauty of forests, mountains and waterways, it is not particularly conducive to car travel. Highways and roads snake up and down and around the landscape in circuitous paths, making navigation an adventure for rural inhabitants, and even treacherous in bad weather conditions.

Clustered in this region are eight freestanding radiotherapy clinics in the communities of Clyde, Franklin, Weaverville, Forest City, Marion, Asheville, Hendersonville and Brevard. GenesisCare inherited these strategically located centers in a May 2020 acquisition.
“Despite our distributed clinic model, getting to the clinic for five days a week treatments is always going to be a challenge due to the geography in this part of the state,” says GenesisCare radiation oncologist Daniel Baseman, MD, who covers Brevard, Asheville and Hendersonville. “As you go west from Brevard in Transylvania County, especially, it’s very mountainous and you’re getting farther away from the closest place one could get radiation. And it’s not just distance. A person’s house might be a little closer to our Franklin clinic, but it’s on the other side of a mountain – no one wants to drive on it.”
Compounding travel difficulties is the number of people without health insurance, with Transylvania County exceeding the national average for uninsured individuals.
“Many patients lack employer-based healthcare and thus are ineligible for Medicare,” he says. “Rural residents are also sometimes less vigilant about getting screening studies and often present with more advanced diagnoses.”
In terms of financing cancer care, all of North Carolina’s GenesisCare centers strive to work with patients with and without insurance to arrive at a solution that is workable for them. A major way to make radiotherapy more affordable is finding opportunities to hypofractionate treatments, Dr. Baseman observes.
“Some patients’ insurance is ‘half co-pay,’ every time they walk into the doctor’s office, so you’re always going to want to consider hypofractionation,” he says. “But an arguably even bigger impact of hypofractionation is, again, transportation issues.”
Dr. Baseman relates the case of a node-negative breast cancer patient who lived in a skilled nursing facility south of the Hendersonville clinic, but who had to rely on her daughter who lived 80 minutes away to bring her to the center.

“A typical three-week radiotherapy course would have been impossible for her due to the travel times, but a five-fraction treatment was very attractive to her and her daughter. In this case, we treated her with partial breast radiotherapy as she met suitability criteria for such therapy,” he says. “We don’t have as much data describing this approach as opposed to more traditional whole breast radiotherapy, but the data we do have is very encouraging, and it’s going to be increasingly employed. It worked great for her – she tolerated the treatment well and we treated her in just five days.”
A major leap in the ability to hypofractionate prostate cases at the Asheville and Hendersonville clinics came with the acquisition of a Versa HD system for each of the centers, Dr. Baseman adds. The linacs went live in January and July 2021, respectively.
“We’ve seen prostate courses go from eight to nine weeks to now five-and-a-half or four weeks to even only five treatments if you utilize extreme hypofractionation,” he notes. “I wouldn’t have tried extreme hypofractionation on a prostate using our previous linacs, because those systems did not have kV cone beam CT-based image guidance nor intrafraction positional tracking. Without capabilities such as these, optimal patient positioning for such high dose therapies is not possible.”
GenesisCare’s distributed network of North Carolina radiotherapy clinics, financial assistance, hypofractionation schemes and more advanced treatment systems have played an outsized role in helping address disparities in cancer care between rural and metropolitan areas, Dr. Baseman adds.
“…Getting the Versa HD systems has begun narrowing the care gap for our rural patients.”
“Our presence dispersed in these eight western communities has really helped lessen the burden on our rural patients, and getting the Versa HD systems has begun narrowing the care gap for our rural patients,” he says. “As we expand and acquire more of these linacs it’s really going to increase what we can offer patients close to home.”
A spectrum of challenges facing rural cancer patients1
- 15-19% of US population live outside major metro centers
- Combined incidence rates for cancer are higher in urban areas, but death rates are higher in rural areas.
- Patients often diagnosed at later stages; are less likely to receive standard of care treatment, follow-up or supportive services; and have worse health outcomes during survivorship than nonrural patients.
- Patients tend to be older, have poorer general health, higher rates of obesity, disability, smoking or drug use, and have lower access to screening and prevention services – leading to higher rates of tobacco related, HPV, lung, cervical and colorectal cancers.
- Lower education, income, differences in health literacy and cultural trust in medical system (i.e., stoicism) – delay doctor visits or skip routine screenings.
- Geographic distribution of services: more spread out and fewer generalist and specialist providers; fewer hospitals and other treatment facilities; fewer dedicated cancer centers; fewer resources, such as labs, or RO services.
- Only 12-15% of oncologists work in rural settings.
- More than half of all US counties have no available oncologist. Counties without oncologists represent 2.2 million sq miles (60 percent of US land area).
- Travel distance and costs: lack of care providers: about 20% of rural Americans live more than 60 miles from a medical oncologist. Costs: travel, meals and lodging, lost time at work or child care demands.
- Financial burdens and health insurance: Rural residents less likely to be covered by work-sponsored health insurance and more like covered by Medicare and Medicaid, or uninsured than urban people.
References
- Levit LA, Byatt L, Lyss AP, Paskett ED, Levit K, Kirkwood K, Schenkel C, Schilsky RL. Closing the Rural Cancer Care Gap: Three Institutional Approaches. JCO Oncol Pract. 2020 Jul;16(7):422-430. doi: 10.1200/OP.20.00174. Epub 2020 Jun 23. PMID: 32574128.
- https://www.ouhealth.com/stephenson-cancer-center/community-outreach-and-engagement/cancer-issues-in-oklahoma/