High-precision, personalized stereotactic radiotherapy for Colorado prostate cancer patients

The Urology Center of Colorado uses comprehensive Elekta solution for effective, short-course stereotactic body radiation therapy (SBRT)
Acquiring a robust suite of Elekta radiotherapy solutions – encompassing beam delivery, patient positioning and treatment planning – is changing the world for prostate cancer patients at The Urology Center of Colorado (TUCC), a dedicated urology center in Denver, USA. The center’s equipment includes an Elekta Versa HD™ linear accelerator, HexaPOD™ evo RT System and Monaco® treatment planning system for high-definition dynamic radiosurgery (HDRS) and Clarity® Autoscan for optimized visualization. This combination enables TUCC to deliver sophisticated, focused prostate radiotherapy techniques – such as VMAT, IGRT and SBRT – all while minimizing the risk of side effects.
The TUCC prostate SBRT protocol is based on NRG Oncology RTOG 09382, a randomized phase II trial of hypofractionated radiotherapy for favorable-risk prostate cancer.
“Before acquiring Versa HD, we weren’t able to consider a protocol such as RTOG 0938.”
“Before acquiring Versa HD, we weren’t able to consider a protocol such as RTOG 0938,” says David Powers, MS, DABR, medical physicist at TUCC. “Due to our previous linac’s limitations, we estimated that treatments would take up to 45 minutes and require re-imaging every seven minutes according to protocol. Such long delivery times would increase uncertainty, which we deemed unacceptable given the high dose per fraction required for prostate SBRT.”
After Versa HD commissioning and adoption of Monaco, TUCC was able to address these concerns, adopting the RTOG 0938 protocol for its prostate SBRT program. The protocol calls for either 5 fractions/7.25 Gy per fraction (total dose 36.25 Gy) or 12 fractions/4.3 Gy per fraction (total dose 51.6 Gy). TUCC opted for shorter fractionation schedule.
“Since we installed Versa HD in 2016, we have treated over 800 patients, of which we used SBRT to treat about 50,” Powers notes. “Of these SBRT cases, 30 were for prostate cancer. The expected side effects have been minimal and there have been no major treatment complications.”
The TUCC prostate SBRT workflow
Patient selection:
Patients are selected for the SBRT program according to RTOG 0938 recruitment guidelines2:
- Within one year of diagnosis
- Low risk (Gleason scores 2-6, clinical stage T1–2a, PSA <10)
- No evidence of distant metastases
- No regional lymph node involvement
- No previous hormonal therapy
- No cytotoxic chemotherapy for prostate cancer
Pre-simulation:
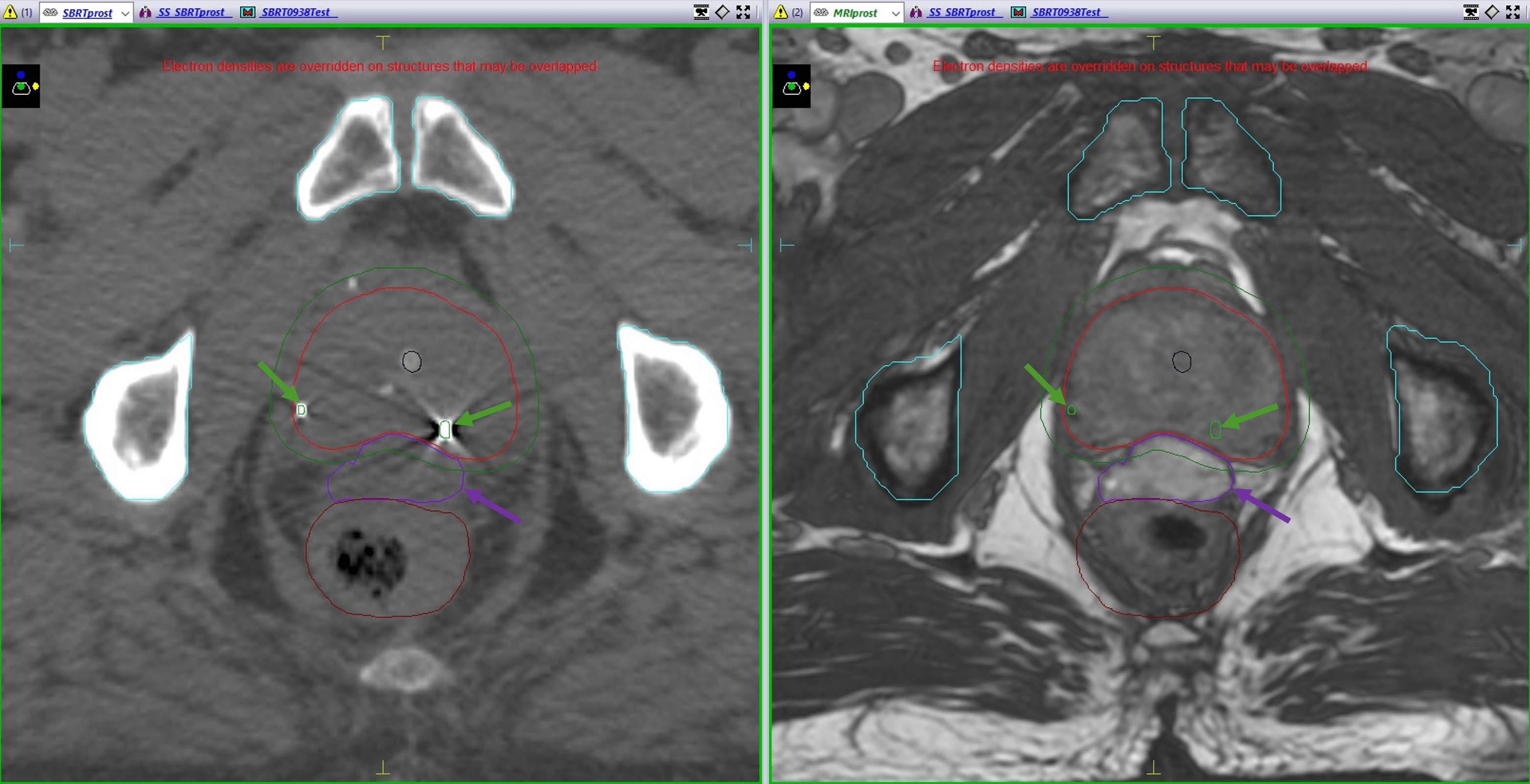
One to two weeks before simulation, clinicians implant three gold fiducial markers into the prostate and inject hydrogel to create space between the prostate and rectum (Figure 1)
Simulation:
TUCC physicians simulate with CT and acquire a Clarity® scan to visualize soft tissues. These images are co-registered later in the software and the isocenter is set. On the same day as CT-sim, a T2-weighted MRI scan is performed with 1-2 mm slices through the prostate.
Planning:
In the planning stage, the CT and MR images are fused. The prostate and hydrogel are contoured on the MR images, while the gold fiducials are marked using the CT images. Treatment planners use Monaco (v 5.11) to develop the plan. The resulting VMAT plan is designed to deliver 7.25 Gy using a 10 MV FFF beam. A single 360ο beam is used, with one to two arcs per beam. PTV margins are 3 mm posteriorly and 5 mm everywhere else (inferior, superior and anterior) according to RTOG 0938 guidelines.2 Constraints also are applied per RTOG 0938 recommendations.2
Quality assurance (QA):
Plan QA is performed using Sun Nuclear ArcCHECK with an ion chamber. The goal is to achieve a 3D gamma analysis pass rate (gamma index < 1) of ≥ 97% with criteria of 2%/2 mm but a pass rate of ≥ 97% with criteria of 3%/3 mm is acceptable.
The ion chamber reading in ArcCHECK must be within 2% of the planned dose. A second MU check is also performed using third-party software and must show less than 3% difference. In addition, machine QA is carried out with a weekly Winston-Lutz isocenter check using Sun Nuclear’s SNC Machine, and daily imaging, shifts, laser and isocenter checks are performed using a Quasar Phantom.
Patient setup and motion monitoring:
Image guidance for patient setup is performed using CBCT and XVI. The daily CBCT image is aligned with planning images using the gold fiducials (Figure 2), and the required couch shifts are made utilizing the HexaPOD evo RT System.
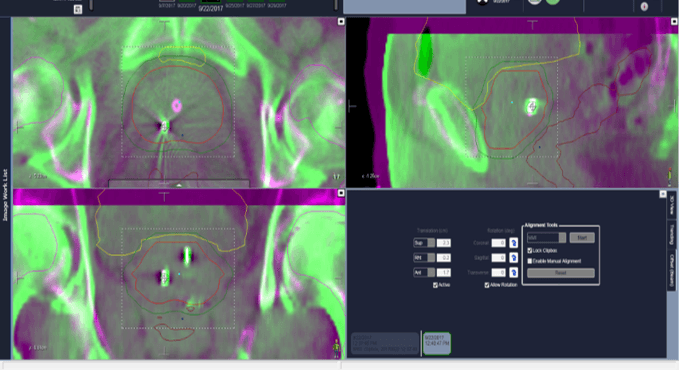
Prostate scanning and tracking begin before CBCT, using Clarity soft tissue monitoring. Clarity helps reduce uncertainty caused by prostate motion by tracking prostate movement during irradiation and allowing gated treatment delivery. This increases delivery confidence and allows the use of smaller margins.
During treatment, if the prostate drifts out of an established threshold, the radiation beam is halted. Treatment resumes when the prostate goes back to position or after manual table adjustments.
Treatment:
Fractions are delivered every other day for five fractions, each fraction taking 10 to 15 minutes.
“This is a vast improvement on what we could achieve with our previous linac, which minimizes opportunities for intrafraction motion and enhances patient comfort,” Power says.
Plan optimization with Monaco
At TUCC, the planning team uses several Monaco features to provide optimal target coverage and sparing of organs at risk (OAR).
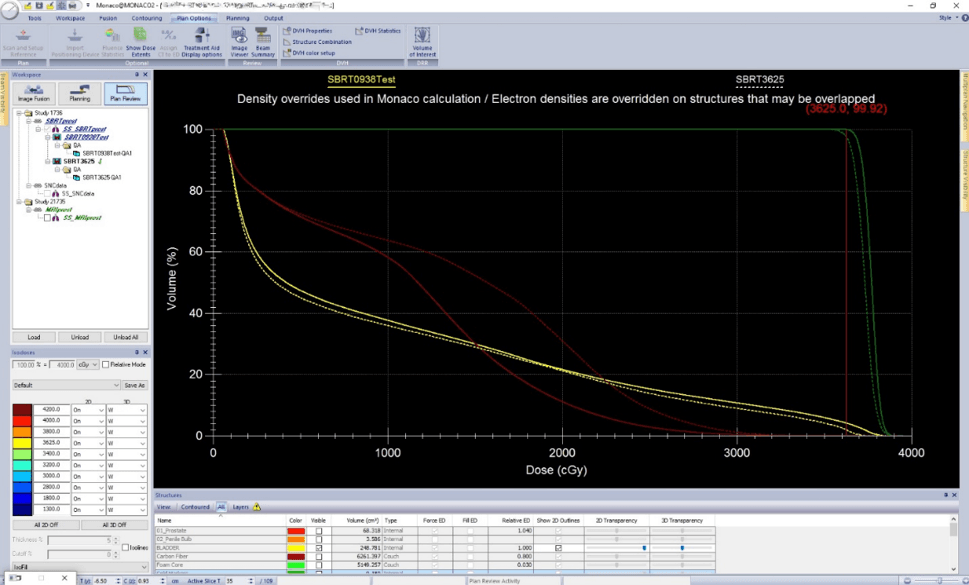
“Multicriterial optimization [MCO] is used with constrained optimization to automatically adjust constraints to achieve better normal tissue sparing while preserving target coverage,” Powers explains. “When OAR doses are met and target cost functions are achieved, MCO is able to drive OAR doses even lower, stopping before target coverage is compromised, to deliver a higher quality plan for the patient.” For the DVH shown in Figure 3, the Red DVH line that represents the Rectum shows increased Rectal Sparing with MCO applied (solid line with MCO).
The Monaco system’s multiple arc-per-beam option allows radiation dose delivery to be optimized using one to two arcs in a single beam, without stopping radiation delivery, he adds. This results in a more efficient VMAT delivery in terms of MU, control points and delivery times, helping to reduce patient time on the table.
“The unique combination of Monaco and Versa HD for HDRS ensures optimum target coverage and maximum OAR sparing.”
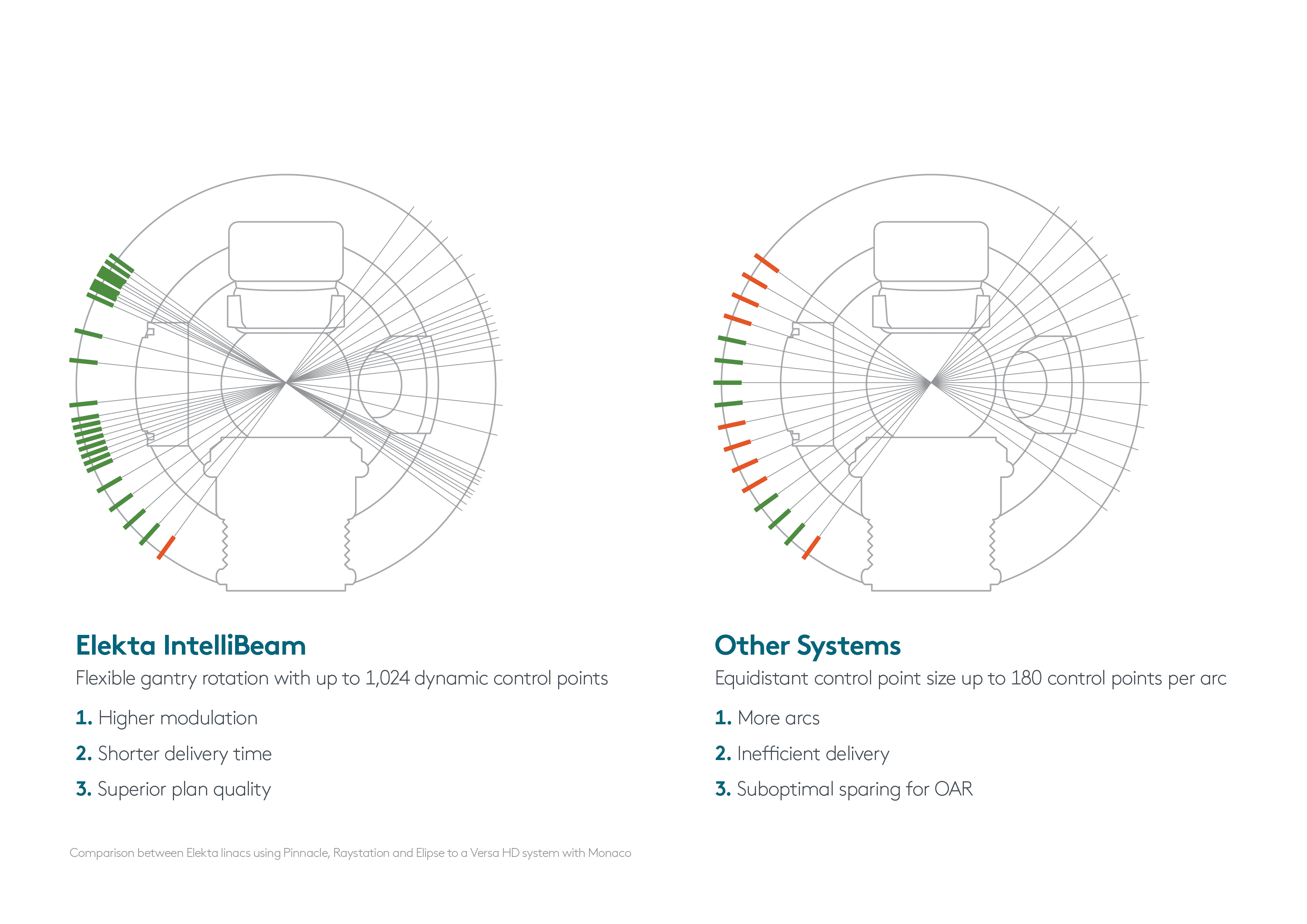
“The unique combination of Monaco and Versa HD for HDRS ensures optimum target coverage and maximum OAR sparing,” he observes. “This excellent plan quality is achieved using a combination of segment shape optimization, higher modulation and the IntelliBeam variable control point size. With less flexibility and fewer control points per arc, other treatment planning systems can’t maximize the Versa HD system’s full capabilities in this way and are likely to require the use of more arcs.” (Figure 4)
An enduring tradition of targeted, personalized prostate SBRT
The accuracy of Versa HD HDRS with Monaco has enabled the TUCC team to use smaller margins and has reduced potential errors.
“Monaco MCO allows a standardized approach to deliver robust personalized treatment plans to our patients,” Powers says. “This has increased our confidence to deliver high doses, and has resulted in shorter treatment times, improved outcomes and reduced side effects for patients. Plus, the ability to deliver prostate SBRT reduces the number of fractions required, which has benefited patients who have to travel far for treatment.”
Following the successful implementation of the TUCC prostate SBRT protocol, the center intends to extend its SBRT program to include additional indications. The Versa HD HDRS solution has enabled the team to treat an inoperable renal cell carcinoma patient with ablative doses successfully.4,5 In addition, TUCC has introduced SBRT for bone metastases and positive solitary local nodes for prostate cancer.
Recent trends in treating prostate cancer
Prostate cancer is among the most frequently diagnosed cancers in men, with approximately 1.3 million new cases diagnosed worldwide in 2018.1 Radiotherapy is a common treatment option for localized disease, with patients conventionally treated daily over seven to eight weeks.2 Recently, there has been considerable interest in hypofractionated radiation therapy regimens for treating prostate cancer, as it offers potential radiobiological advantages and patient convenience benefits.2,3
The ability of modern high-precision radiotherapy techniques to deliver hypofractionated treatment regimens for prostate cancer with a low incidence of side effects has been recognized.3 A recent phase II randomized multicenter trial (NRG Oncology RTOG 0938) was designed to assess quality of life outcomes and toxicity (acute and late) for two different hypofractionated regimens: 36.25 Gy delivered in 5 fractions of 7.25 Gy twice a week, and 51.6 Gy delivered in 12 daily fractions of 4.3 Gy.2 In this study, the urinary and rectal quality of life outcomes reported by patients with prostate cancer undergoing hypofractionated radiation therapy (5 or 12 fractions) were shown to be comparable to those with standard fractionation regimens.3
References:
- Globocan 2018. https://www.uicc.org/news/new-global-cancer-data-globocan-2018
- NRG Oncology, RTOG 0938 protocol. A randomized phase II trial of hypofractionated radiotherapy for favorable risk prostate cancer.
- Lukka HR, Pugh SL, Bruner DW, et al. Patient reported outcomes in NRG oncology RTOG 0938, evaluating two ultrahypofractionated regimens for prostate cancer. Int J Radiat Oncol Biol Phys. 2018;102(2):287-95. DOI: 10.1016/j.ijrobp.2018.06.008
- Pham D, Thompson A, Kron T, et al. Stereotactic ablative body radiation theray for primary kidney cancer: A 3-dimensional conformal technique associated with low rates of early toxicity. Int J Radiat Oncol Biol Phys. 2014;90(S):1061-68.
- Pham D, Kron T, Bressel M, et al. Image guidance and stabilization for stereotactic ablative body radiation therappy (SABR) treatment of primary kidney cancer. PRO. 2015;5:e597-605.





