Growing wave of elderly cancer patients emphasizes need for personalized treatments
The Sidney Kimmel Cancer Center at Jefferson Health’s Geriatric Oncology Center of Excellence and Senior Adult Oncology Center ensure older individuals receive world-class care
Advanced age is a well-established risk factor for cancer and the number of people entering the ranks of the “elderly” (i.e., 65+) is rising like a tidal wave. The National Cancer Institute projects that by 2040, three out of four US cancer survivors will be older than 65.1-2 Dr. Andrew Chapman and his colleagues at the Sidney Kimmel Cancer Center – Jefferson Health (SKCC) refer to this cancer-related demographic trend as the “silver oncologic tsunami.”3 Fortunately, because Dr. Chapman and his teams noticed this swell building a while ago, the Jefferson Senior Adult Oncology Center (SAO) was established in 2010, and in 2022, the Geriatric Oncology Center of Excellence, which the SAO Center folds into.
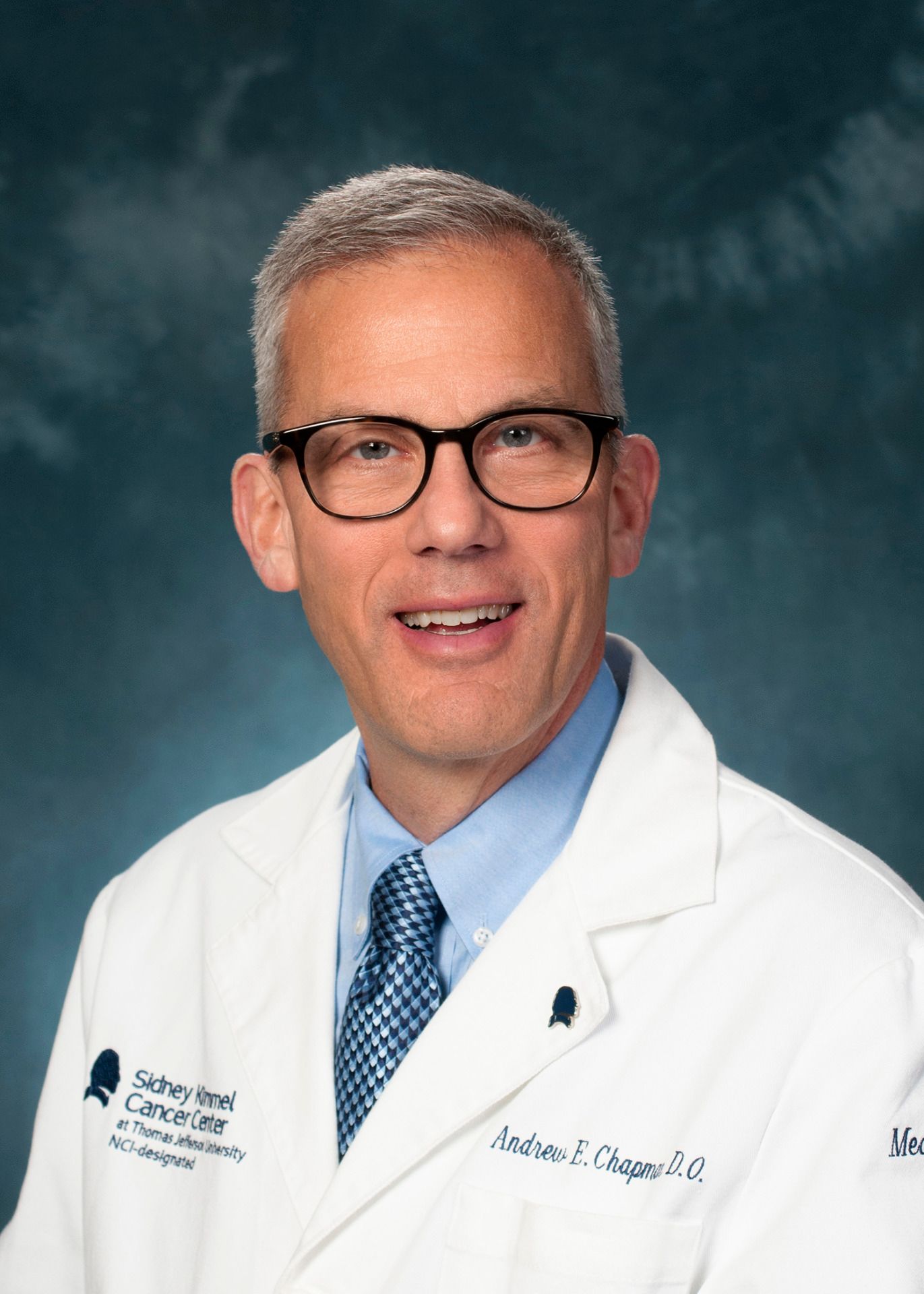
“What was apparent to me in 2010 was that healthcare delivery in the United States and in many other countries was fragmented and costly,” says Dr. Chapman, DO, FACP, FCPP, a medical oncologist and SKCC director, and co-founder and co-director of the SAO. “I began to realize that older adult cancer patients were at the greatest risk of falling through the cracks in care delivery models. So, to better assess an older cancer patient’s needs and goals we needed to do a much better evaluation of those patients – beyond standard performance status measures or a patient’s appearance, both of which are notoriously inaccurate.”
For over a decade, the SAO’s clinical care delivery model – now one of the five pillars of the Geriatric Oncology Center of Excellence (see sidebar) – has enhanced the access, quality and delivery of specialized cancer care that focuses on aspects affecting older adults.
A different treatment approach for seasoned patients
According to Dr. Chapman, accommodating older cancer patients starts with the recognition that their goals may be vastly different than those of younger patients.
“Often, the most important thing for older adults is maintaining their independence and quality of life and not having those deteriorate as a result of treatment.”
“Curing the disease of elderly patients to help them live 30 or 40 years longer may not be their primary consideration,” he says. “Often, the most important thing for older adults is maintaining their independence and quality of life and not having those deteriorate as a result of treatment.”
After appreciating the older adult cancer patient’s treatment goals, SKCC clinicians deal with the much more complex issues of treating older patients versus younger patients, including cancer biology differences, comorbidities, multiple medications and aging-related physiological changes and how these affect how cancer treatments work.
“Comorbidities may affect how they tolerate therapy and older patients generally have polypharmacy [i.e., > 5 medications], which can interact with the treatment, and there may be adverse drug reactions, as well,” Dr. Chapman explains. “There are also geriatric syndromes, such as falls, incontinence and delirium – all the therapies we give these patients may make those syndromes more pronounced.
“In addition, in older adults there is a high incidence of malnutrition,” he adds, “which can affect the amount of protein in the body, in turn influencing the distribution of protein-bound drugs.4 The bottom line is the margin for error is much narrower in the older adult. You have to be very cautious about what you’re doing and clearly understand what you’re trying to achieve.”
Multidisciplinary team focuses attention on older adult cancer patients
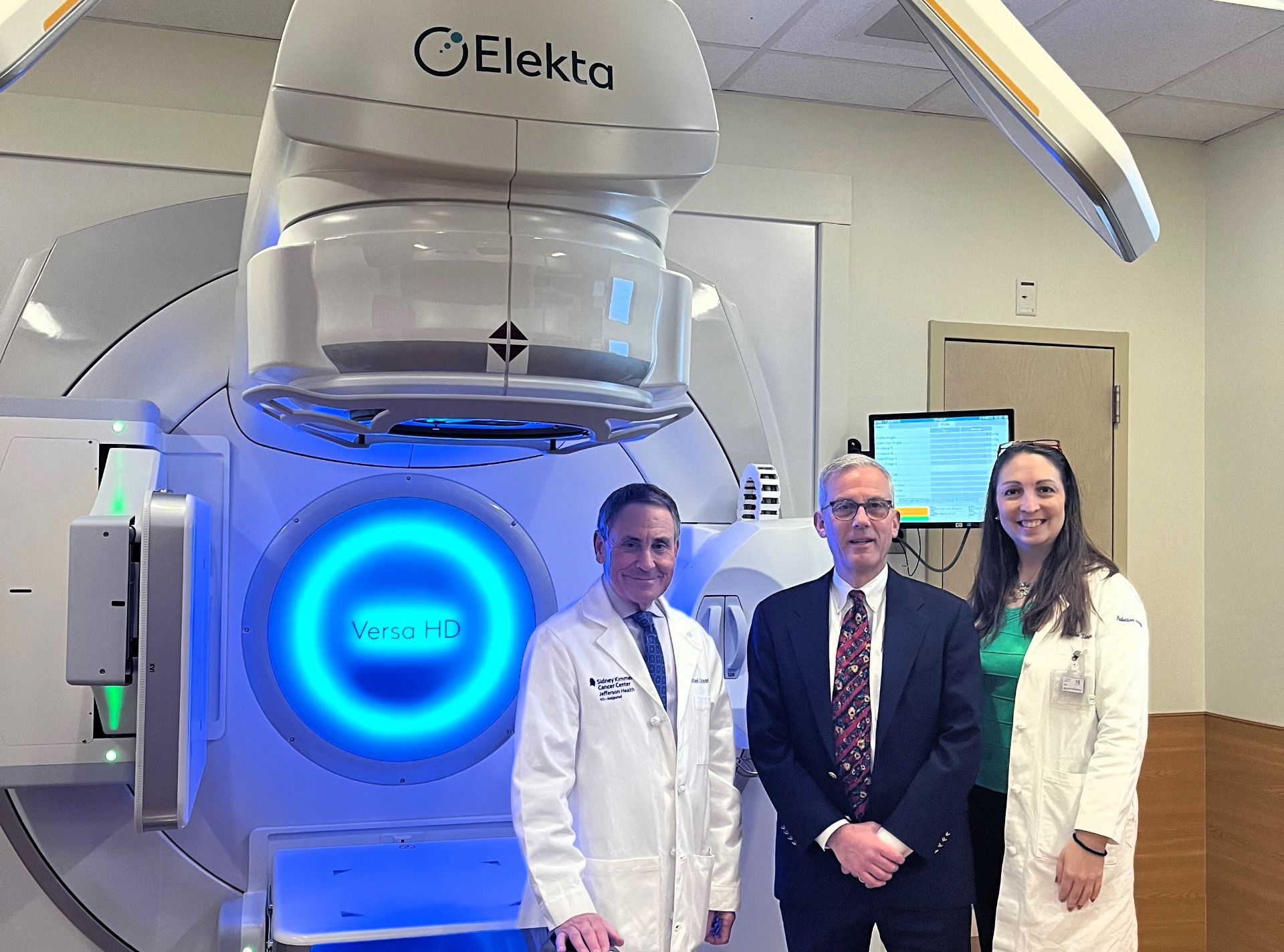
The SAO consolidates several specialties into a multidisciplinary team (MDT) that analyzes each patient’s health status and readiness for cancer therapy. Professionals in geriatrics, medical and radiation oncology, social work, pharmacy, nutrition, and navigation perform a comprehensive geriatric assessment to better understand the patient’s needs.
“When patients enter the clinic – hopefully with their primary caregiver accompanying them – each MDT member rotates in and out of the exam room to consult with each patient, or alternatively, we can do the same thing virtually via telemedicine,” Dr. Chapman says. “While acknowledging the patient’s personal treatment goals upfront, we then sit down in a case conference and review as a group the specific issues about the patient and start recommending how to tailor the therapy – if we should avoid a certain treatment versus another or put in place things like nutritional counseling or physical therapy.”
The MDT characterizes each patient as “fit,” “vulnerable,” or “frail,” based on meticulous testing encompassed in the geriatric assessment.
“We think of this type of geriatric assessment as the greatest form of personalized medicine.”
“Most patients fall into the ‘vulnerable’ category, where with certain manipulations – whether it’s chemotherapy/radiation therapy dose intensity or one specific drug versus another, or adding physical therapy or closer monitoring of an aspect of the patient’s health – we’ll be able to give the patient the therapy he or she wants. We think of this type of geriatric assessment as the greatest form of personalized medicine.”
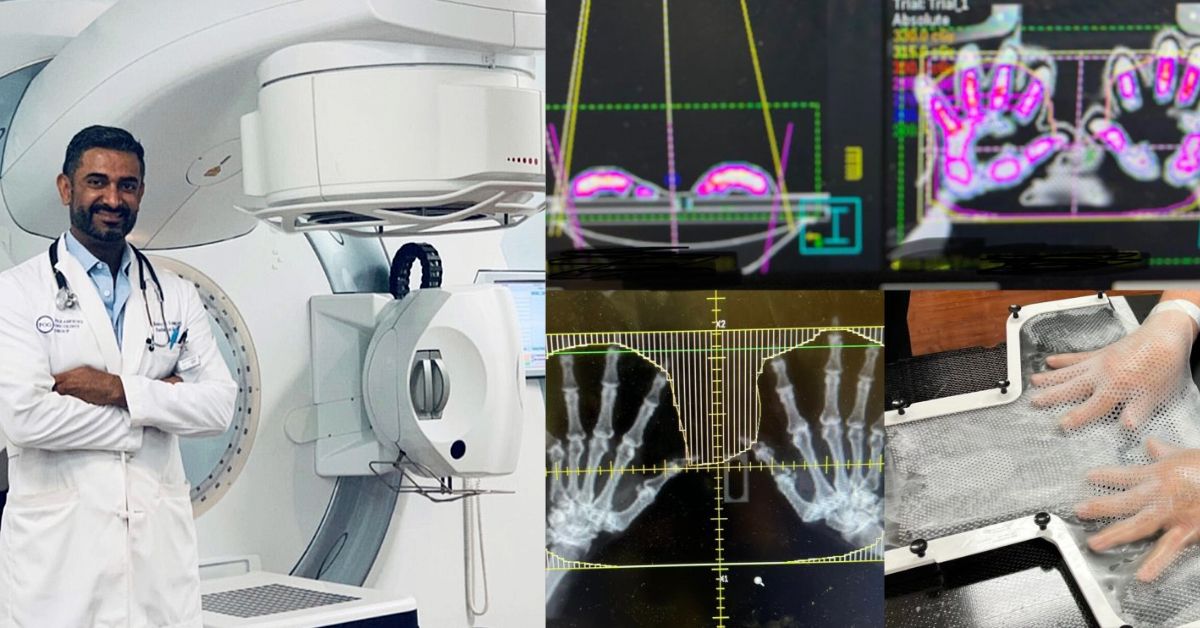
Radiation therapy: a common option
More than half of all cancer patients worldwide will receive radiation therapy as part of their treatment.5 Fortunately, advances in radiotherapy practice and technology have made treatments less arduous than other therapies.
“Sometimes we change doses or the areas that we are going to treat, but most elderly patients do quite well with radiation.”
“There should be a multidisciplinary decision to ensure the older patient is fit and able to undergo radiation therapy,” says radiation oncologist Nicole Simone, MD. “Sometimes we change doses or the areas that we are going to treat, but most elderly patients do quite well with radiation. Although there are some cases in which we may reduce dose, it is not commonly done.”
According to her colleague, radiation oncologist Michael Greenberg, MD, beyond the older patient’s fitness for radiotherapy is whether immediate treatment is necessary.
“For example, for a 70-year-old with precancerous breast cancer, we may just put her under surveillance,” he says. “And there are new genomic markers – their DNA input – that inform us about a patient’s cancer risk. If the results say low-risk we can do active surveillance, but sometimes when it looks like low-risk, but the genomics are high-risk, we recommend radiation therapy.”
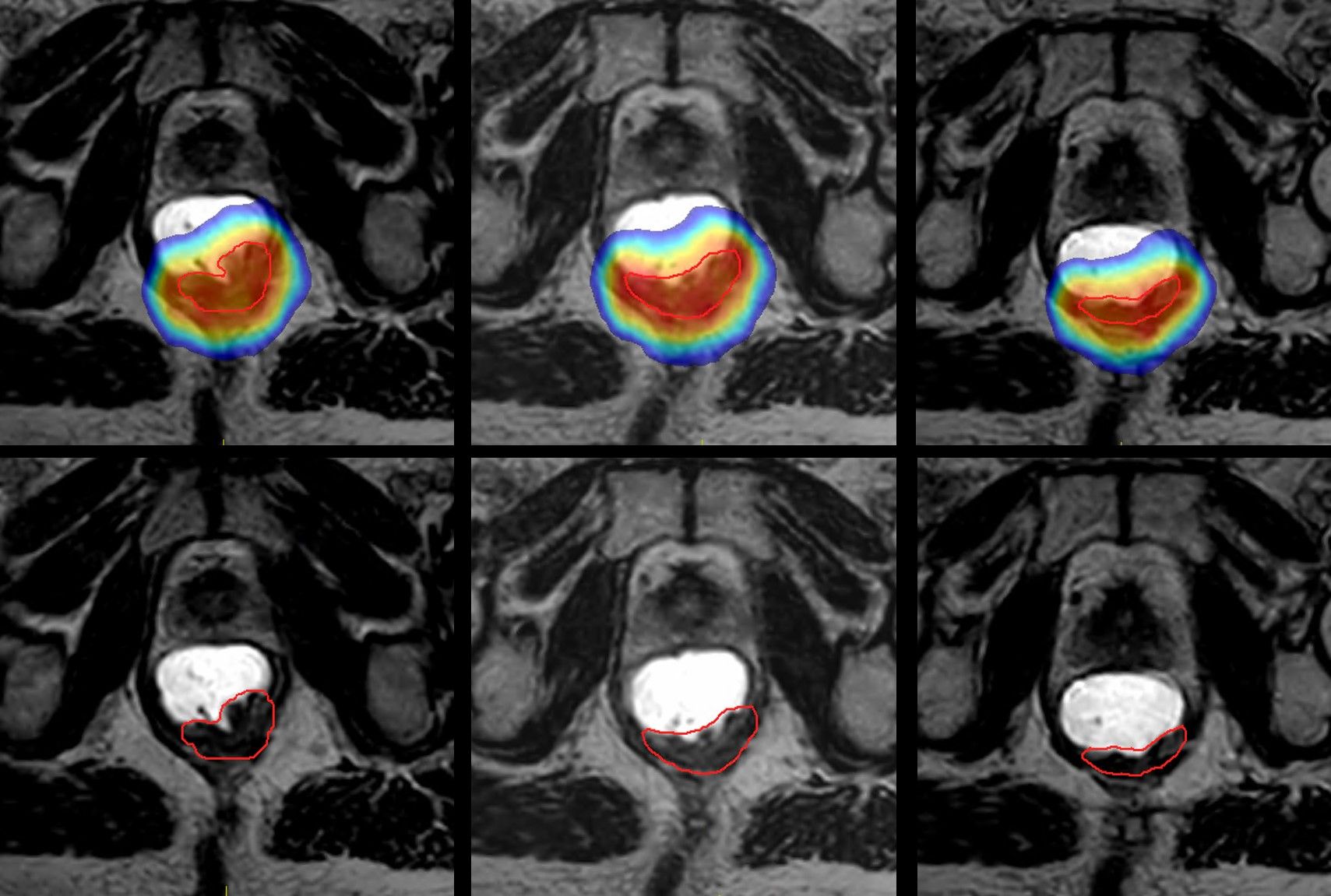
Radiotherapy technology advances have benefited patients of all ages. Prostate cancer radiation therapy, for instance, used to take up to nine-and-a-half weeks, but now can be treated definitively in just five treatments through high-dose hypofractionation. And more precise targeting of cancer with treatment techniques such as stereotactic radiosurgery with Gamma Knife® and MR-guided radiation therapy (MRgRT) with an MR-Linac spare healthy tissues, resulting in fewer side effects.
In caring for elderly patients, decisions on whether to treat or surveil and which therapy to use – surgery, chemotherapy, radiation, or other treatment – are made in SAO’s MDT. Drs. Simone and Greenberg view comorbidities and socioeconomic factors as key determinants.
Comorbidities, as opposed to chronological age, are what physicians focus on, Dr. Simone stresses.
“When I first consult with a patient who is 82 years old, for example, my first thought is: ‘Does this look like an 82-year-old?’,” she says. “I assess their functional age and performance status as measured by KPS or ECOG scores to determine how they will tolerate a given treatment. Patients that are obese, diabetic or those with metabolic dysregulation tend to have worse outcomes with radiation and may have increased toxicity.
“That said, I don’t dose-reduce very often in older patients since most treatment courses we offer have gotten substantially easier to go through, with better preservation of quality of life due to shorter courses of radiation and better technology. If I assess that they can get through treatment, I treat our older population just like everyone else,” Dr. Simone adds. “When Dr. Chapman and I looked at our radiation database of older adults for toxicities like neutropenia, we found there was no additional toxicity.”
An exception is whole brain radiation, in which patients can experience somnolence (daytime sleepiness) or fatigue. Often, these patients are considered for dose reduction, she says. Dr. Greenberg cites socioeconomic factors as a significant consideration in geriatric assessments.
“Some elderly patients are affluent, healthier on average, have better diets and medical care, and go to the gym, while others don’t have the resources to get to the doctor, or need to choose which medications they get because they can’t afford the co-pay,” he says. “In the MDT we need to identify these issues among our older patients and see if we can provide financial assistance or other accommodations.”
Shared decision-making should be the standard of care for older adult patients
Comorbidities, socioeconomic issues, the inherent vulnerability of older patients and appreciating their desires make shared decision-making the primary driver for treatment planning, according to Dr. Chapman.

“This means considering what is important to the older adult and not doing what used to happen years ago, which was giving the 30-year-old and the 70-year-old the same therapy for the same disease – and not scrutinizing the factors that differentiate the two age groups,” he says.
SKCC’s MDT is very much in line with the guidance of professional groups concerning older adult cancer patients. Medical organizations, such as the American Society of Clinical Oncology (ASCO), the International Society of Geriatric Oncology and the Cancer and Aging Research Group all have endorsed ASCO’s updated guidelines regarding the implementation of the practical geriatric assessment (PGA), a mostly patient self-administered questionnaire to obtain more information upfront.
“We’re going to build the PGA into our EHR so that before the patient even starts therapy, we have the data we need to determine whether the patient would benefit from our MDT geriatric assessment or referral for interventions such as nutrition counseling or physical therapy,” Dr. Chapman says. “We’ve already developed software called the Geriatric 8 (G8) that we use as a screening tool to determine who is fit and who is not.”
Patients deemed unfit would then undergo the ASCO’s practical geriatric assessment. “For a patient with gait issues, for example, we could recommend physical therapy, or for an individual at risk of malnutrition, we could suggest nutrition counseling,” he says. “However, there will be a subset of patients that are going to have such great needs that our MDT’s comprehensive geriatric assessment would be the next step for these patients.”
Patients appreciate SKCC’s care
A cancer diagnosis is unwelcome news for a person of any age; the challenges are magnified when the patient is elderly. However, at a center like SKCC, older adult patients are comforted by the “all-hands-on-deck” attention to their case.
“We were surveyed about the performance of the MDT that was done internally and we scored incredibly high in terms of how well-functioning the team is,” Dr. Chapman says. “We also have scores of anecdotal responses from patients and their caregivers.”
One of Dr. Chapman’s most notable anecdotal responses was from the British daughter-in-law of an American patient.
“…this woman – in her wonderful British accent – burst into tears and told me: ‘The Queen of England could not have gotten care this amazing – thank you!’”
“I was the last member of the MDT to meet with the patient and daughter-in-law, and this woman – in her wonderful British accent – burst into tears and told me: ‘The Queen of England could not have gotten care this amazing – thank you!’”
Addressing the entire cancer continuum for older patients: the five pillars of the SKCC’s Geriatric Oncology Center of Excellence
To address the effects of a cancer diagnosis and treatment in older individuals, each pillar will have a specific focus.
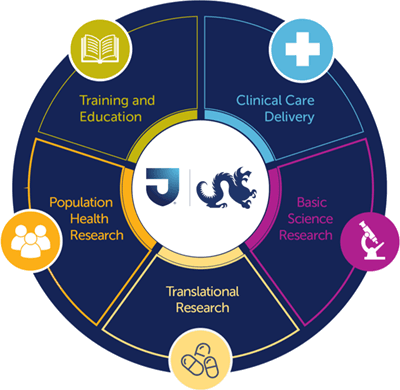
- Basic science research that will explore the aging-associated molecular changes that contribute to cancer susceptibility, progression, and metastasis;
- Translational research that will turn the discoveries uncovered by the basic science arm into novel therapies and clinical trials for a population that has been historically underrepresented in clinical trials;
- Population health research that will provide a better understanding of the underlying drivers of cancer disparities;
- Clinical care delivery, which will improve the access, quality, and delivery of specialized cancer care that focuses on factors impacting older adults; and
- Training and education that will provide significant opportunities to increase the number of specialists and caregivers capable of caring for older adults with cancer.
References
- Laconi E, Marongiu F, DeGregori J. Cancer as a disease of old age: changing mutational and microenvironmental landscapes. Br J Cancer. 2020;122(7):943-952. Epub 2020 Feb 11.
- Dangi-Garimella, S. NCI Predicts a “Silver Tsunami” of Cancer Survivors by 2040, 75% Will Be Over 65. The American Journal of Managed Care. Published July 11, 2016. Accessed February 24, 2023.
- Chapman A, MacKenzie A, Parker I. Silver oncologic tsunami: quality issues in the senior adult oncology population. JCO Oncol Pract. 2015;11(3):190-192.
- Lombardo J, Schmucker AM, Keith SW, et. al. Markers and associations of nutrition identified in a senior adult oncology clinic. J Geriatr Oncol. 2023 Jan;14(1):101388. doi: 10.1016/j.jgo.2022.10.003. Epub 2022 Oct 14. PMID: 36253248.
- https://www.who.int/news/item/05-03-2021-new-who-iaea-publication-provides-guidance-on-radiotherapy-equipment-to-fight-cancer
LARNPS240402