Cyprus clinic reaping the rewards of greater SRS positioning freedom

German Oncology Center’s HexaPOD evo RT system supports sub-millimetric precision in intracranial stereotactic radiosurgery cases

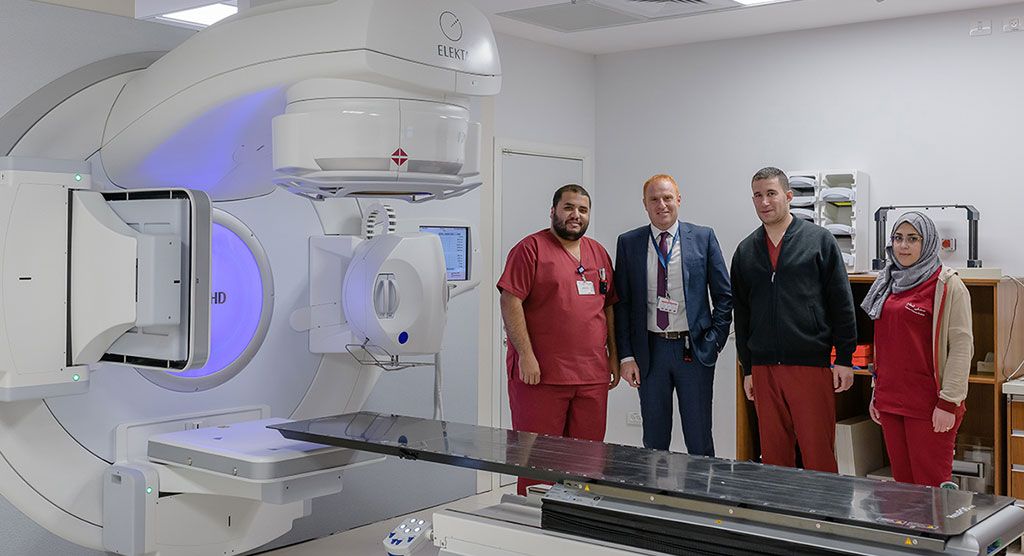
Cyprus’s German Oncology Center (GOC, Agios Athanasios, Limassol) invested heavily three years ago to equip itself with all the advanced systems needed for world-class radiotherapy and radiosurgery, including an Elekta Versa HD™ linac, a HDR brachytherapy afterloader, planning CT and PET/CT systems, an MRI and even a small cyclotron. However, because clinicians couldn’t predict their stereotactic radiosurgery (SRS) volume, they postponed acquiring the Elekta HexaPOD™ evo RT robotic positioning system. It took GOC’s 2018 participation in an SRS end-to-end accuracy study to convince GOC clinicians to put acquisition of HexaPOD on the fast track. Today, GOC routinely performs HexaPOD-supported single isocenter, multi-metastases SRS with exceptional precision.
GOC began its SRS program in late 2017 with the Elekta iBEAM® evo Couchtop as the patient support. Correcting for rotations was challenging, according to Paul Doolan, PhD, GOC General Coordinator of Medical Physics.
“Each of our stereotactic patients has a daily CBCT and we make the CBCT match to determine what patient position translations and rotations are required,” he explains. “However, pre-HexaPOD, we weren’t able to apply the rotations. When the required rotations were more than three degrees, we would re-setup the patient and re-CBCT. When the necessary rotations were less than three degrees, we would make the CBCT match by manually setting the rotation to zero and making the best possible registration.
“We were satisfied with the accuracy and precision following these corrections,” Dr. Doolan continues, “but you can imagine the time it took to set up the patient. It really wasn’t optimal.”
Before HexaPOD, GOC clinicians would be wary of using a single isocenter for multiple-metastasis SRS because they were unable to correct for small rotations; a distant met could be missed completely. The standard at GOC for multiple mets SRS was to use several isocenters.

“For mets that were too far apart or if the mets were too small we had to use multiple isocenters to ensure we were hitting the target,” he says. “The impact of this before treatment was we had to use a different treatment plan, different QA and different countersigning procedures for each treatment isocenter. During treatment we had to repeat the shift from the tattoos to the treatment isocenter, the CBCT acquisition and the 3D translations for each metastasis.”
“That meant longer treatment times and the planning was quite tricky, because we needed to account for the beam directions so they don’t overlap too much when treating the different mets,” Dr. Doolan adds. “The time taken to set up, CBCT, make moves and treat is around 10 to 12 minutes, because we usually treat these mets with four beams, three of which are non-coplanar. So, it required the RTTs to go into the room and move the couch between fields 1 and 2, between 2 and 3, and between 3 and 4.”
GOC managed with their multiple-isocenter patient positioning protocol for 21 months, until the clinic began using HexaPOD in June 2019. The impetus to acquire HexaPOD as soon as possible was GOC’s participation in a multi-center validation study of an innovative new RTsafe (Athens, Greece) phantom for verifying end-to-end SRS accuracy.
Validating the RTsafe PseudoPatient Prime phantom
An opportunity arose for GOC in December 2017 to contribute to a multi-center study to validate a prototype of the RTsafe PseudoPatient™ Prime phantom in the clinical setting. Coordinated by RTsafe and University of Texas Health Science Center (San Antonio, Texas, USA), the study enlisted six centers, all of which used Versa HD™, the system’s Agility™ MLC, Monaco® treatment planning and HexaPOD. GOC was the seventh center.
“Although we didn’t have HexaPOD installed during that time, we expressed our strong interest in participating in the validation study, in order to compare ourselves to centers with a vast experience in SRS/SRT treatment around the world,” says Georgios Anagnostopoulos, PhD, former Head of the Medical Physics Department at GOC.
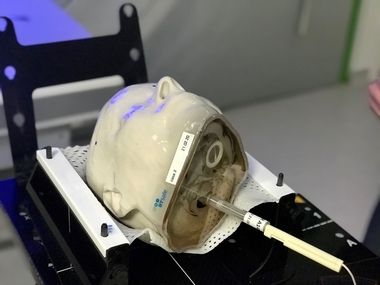
Each site received head phantoms (ion chamber, gel and film) and a patient-derived CT dataset that included a set of structures to plan on. The centers acquired a CBCT scan of the phantom which was registered with the planning CT to ensure agreement. They treated the phantoms as if they were the patient.
According to Dr. Anagnostopoulos, the GOC point dose measurements with the ion chamber showed very good agreement with the results of the six other centers, with a standard deviation across all centers within 2%. Furthermore, the dosimetric 2D film analysis with a %DD/DTA of 3%/2mm (dose threshold value 20% of the prescribed dose) exhibited a gamma passing rate of approximately 98%. Therefore, GOC’s dosimetric accuracy, with the aid of ion chamber point and GafChromic 2D measurements, was verified.
“Conversely, the 3D gel dosimetry conducted by RTsafe revealed that with decreasing target diameter and with increasing distance from the isocenter, our rotational errors contributed to larger dosimetric discrepancies than the other centers,” he notes. “For example, for a 21-millimeter target with a three centimeter distance from the isocenter, our gamma index passing rate was 8.5% less than the average value of the sites that used HexaPOD.”
Dr. Anagnostopoulos asked RTsafe to reevaluate GOC’s gel dosimetry measurements by providing them with the rotational values from XVI CBCT system, in order to correct for positioning misalignments.
“The multi-center study reaffirmed the advantages and the critical need for HexaPOD 6DofF [six degrees of freedom] corrections.”

“RTsafe performed this test and we could see that the results improved significantly by correcting the rotational head phantom positioning discrepancies,” he says. “The multi-center study reaffirmed the advantages and the critical need for HexaPOD 6DofF [six degrees of freedom] corrections. By replacing the iBEAM couch with HexaPOD we could extend our ability to treat multiple brain metastases with a single isocenter. Other factors–such as the time difference in making position adjustments and the reduction of target margins–contributed to the decision to replace our existing patient support.”
After the study results were reported in March 2018, Dr. Anagnostopoulos, GOC’s Medical Director Professor. Dr. Dr. Zamboglou, and Head of Radiation Oncology Dr. Konstantinos Ferentinos decided to acquire HexaPOD. After discussions with the GOC board of directors and Elekta, HexaPOD was installed in June 2019.
Zeroing in on mets with HexaPOD

GOC has been using HexaPOD now for over one year, with mets the vast majority (90-95%) of intracranial SRS cases. (Extracranial SBRT cases include hypofractionated treatment of lungs, abdominal lymph nodes, bones and prostate.) Among the mets cases is a preponderance of patients with multiple mets, for whom the preferred and most often employed SRS treatment technique is the use of a single isocenter. To perform these treatments with the utmost precision and efficiency, HexaPOD with its six degrees of positioning freedom has been indispensable.
“We are much more confident using a single isocenter now, knowing that we’re delivering the dose correctly.”

“We are much more confident using a single isocenter now, knowing that we’re delivering the dose correctly,” Dr. Doolan says. “The size of the mets can be very small, regularly less than 1 cc. If the isocenter is on a single met, then rotation is not going to have a significant impact. However, when there are multiple mets separated by a reasonably large distance–say, greater than 4 centimeters–you really need to be able to apply the rotations. If you can’t, then it’s possible to miss the met completely. Before HexaPOD, we wouldn’t have been confident to use this approach unless the mets were large or the distance between them was less than 4 centimeters.”
The benefits for patients with multiple metastases are clear, he adds.
“For each additional met that we treat with a single isocenter we save around 10 to 12 minutes of time for the patient on the bed.”
“Not only do we know that we’re hitting every metastasis exactly the way we want to, but the length of time the patient will spend on the treatment table, inside a stereotactic thermoplastic mask, is also reduced,” Dr. Doolan says. “For each additional met that we treat with a single isocenter we save around 10 to 12 minutes of time for the patient on the bed. I think patients would accept longer treatment times if it meant a more accurate treatment, but the fact that they’re getting more accurate therapy as well as a shorter treatment time makes things doubly beneficial for them.”
Ongoing collaboration with RTsafe reinforces HexaPOD accuracy
To regularly assess the geometric and dosimetric end-to-end accuracy of GOCs SRS/SRT treatment chain, the Cyprus center is continuing to work with RTsafe.
In the collaboration, selected intracranial patients undergo additional QA tests. Their CT scan is anonymized and converted into a 3D model – with specifications about at least two locations (i.e., tumor target and nearby OAR) that should be measured – and delivered to RTSafe. The company subsequently creates and returns to GOC a 3D printed model within 48 hours.
“We take the 3D printed head and set it up in the patient’s immobilization and acquire the CBCT using the protocol that would be employed for the patient – basically it’s everything that would happen if the patient was here,” Dr. Doolan explains. “After the CBCT, we make the match, apply the table corrections, including the rotations now that we have HexaPOD. Then, to evaluate the precision of HexaPOD, we do another CBCT and repeat the match.
“When we do that, we find that the table shifts are almost always less than 1 millimeter and less than 1 degree,” he continues. “So, we can be confident that we’re setting up with that kind of precision. It really contributes to our peace of mind that we’re providing the patient that level of accuracy.”