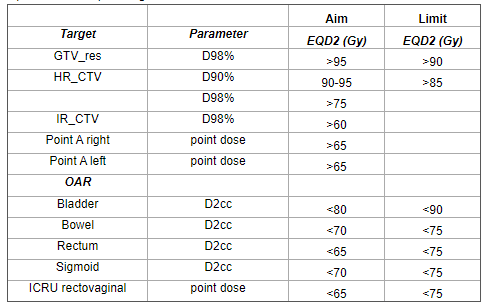
Clinic’s new GYN applicator boosts cervical cancer brachytherapy capabilities

Netherlands medical center harnesses Geneva Universal Gynecological Applicator designed to benefit the majority of patients with locally advanced cervical cancer

Clinicians at Leiden University Medical Center (LUMC, Leiden, The Netherlands) recently began using their new Geneva applicator for patients with cervical cancer up to stage IIB, which represents the majority of patients worldwide with locally advanced disease. Geneva – with its variety of ovoid sizes and interstitial needle positions, as well as several other features – has proven to be a welcome complement to the Venezia™ Advanced Gynecological Applicator the center acquired in 2017 for patients whose cancer has spread to the parametrium and beyond.
“We needed to replace our Utrecht applicators as they were beyond life expectancy,” says radiation oncologist Laura Velema, MD at LUMC, Europe’s first center to use Geneva clinically. “We thought that the Geneva applicator would be an attractive addition to our applicator selection due to its options for ovoid sizes and needle positions. Geneva has a 13 mm ovoid size that is more suitable for patients with smaller anatomy, and the larger Geneva ovoids have medial needle positions that Venezia doesn’t, which makes these Geneva ovoids practical for ventral/medial tumors, and also for recurrent tumors on top of the vagina.
“Another Geneva innovation is the reduction in the intrauterine tubes’ offset from 12 mm to 8.3 mm, which enables us to load the active source closer to the fundus when needed.”
“Another Geneva innovation is the reduction in the intrauterine tubes’ offset from 12 mm to 8.3 mm,” she adds, “which enables us to load the active source closer to the fundus when needed.”
In January 2021, Dr. Velema and her team began using Geneva for post-EBRT boost according to the EMBRACE II protocol (Figure 1). At the beginning of March 2021, LUMC had treated three patients using Geneva.

The first patient was a 63-year-old with FIGO IIB cervical carcinoma.
“She had parametrium invasion on the left, but had very good regression, so in the end we were able to satisfy the EMBRACE II goals with two applications and three fractions instead of four due to the very nice dose distribution,” she says. The treatment entailed 20 mm ovoids, 50 mm intrauterine tube and six interstitial needles (four needles 1st application, two needles 2nd application).
Clinicians treated the second patient, a 46-year-old with FIGO IIIC2 (T2bN1), whose first application was with Venezia and the second application with Geneva, employing six interstitial needles in the second application only.
“The reason we switched to Geneva for the second application was that Venezia needle positions in the 26 mm ovoids are wider, so the needles tend to arrive in the parametrium more laterally than the tumor,” Dr. Velema says. “So, in that case the Geneva needle positions in the 25 mm ovoids enabled us to insert the needles well into the high-risk CTV closer to the central axis of the applicator rather than more peripheral to it.”
The third patient was a 54-year-old with FIGO IIIC cervical carincoma [T2bN1], whose two Geneva applications involved 13 mm ovoids and seven needles (four needles 1st application, three needles 2nd application).
“This patient had a narrow vagina, which required the smallest applicator possible,” Dr. Velema observes. “Therefore, the 13 mm ovoids of Geneva were more suitable in this case than the larger Venezia ovoids.”
Geneva assessment so far
While still in their early weeks of Geneva use, the LUMC team has some informed observations about certain aspects of the applicator.
Commissioning
According to LUMC Medical Physicist Ellen M. Kerkhof, PhD, Geneva commissioning went smoothly for both intrauterine tubes and ovoid tubes, but she offered some advice on commissioning the 13 mm ovoids.
“These smallest ovoids are not loose components, they have their own fixed ovoid tubes,” she says. “To measure the offset of the most distal dwell position, usually you place only the ovoid tube – and not the ovoid itself – on film. It’s different with the 13 mm ovoids. The distance to the film is increased due to the integrated ovoids, which increases the measuring uncertainty a bit. However, with Elekta and Radboud UMC in Nijmegen, we are working on a white paper on Geneva commissioning to make the process more efficient.”
Reconstruction using applicator modeling
LUMC radiotherapy technologist Heloisa Deuzeman found this process “very convenient and straightforward.”
“Because an assembled Geneva has a fixed geometry, the applicator can be reconstructed as a whole and the individual ovoid and intrauterine tubes do not have to be moved or rotated with regard to each other,” she observes. “Before we brought Geneva into the clinic we took the time to design standard library plans for all combinations of intrauterine tube length and ovoid size, as we do at LUMC for all new applicators. The library plans include normalization, activated dwell positions and dwell weights, right and left point A, vaginal points, number of fractions and prescribed dose.
“Library planning is useful as a starting point. It facilitates later individual optimization that we perform according to a particular patient’s target volume and organs at risk.”
“Library planning is useful as a starting point, Deuzeman adds. “It facilitates later individual optimization that we perform according to a particular patient’s target volume and organs at risk. Overall, library planning improves plan quality and decreases planning discrepancies between RTTs, resulting in more consistent treatment plans independent of the planner’s planning style or skill level.”
Needle path
Dr. Velema notes that differences in the orientation of applicator elements between the Venezia and Geneva devices should be appreciated, as they have a bearing on needle path (Figure 2).
“In Venezia, the needles are parallel to the 30-degree intrauterine tube and in Geneva they go slightly more dorsally, because they follow the curve of the ovoids,” she explains. “We recommend doing a dry run with Geneva to determine the default/ideal needle path.”
Handling
According to Dr. Velema, Geneva is “very easy to use because of the click-together system, which requires just four clicks to assemble, which is different from the screws needed to assemble our former applicators. Our medical resident could place the applicator in the first patient’s second application.”
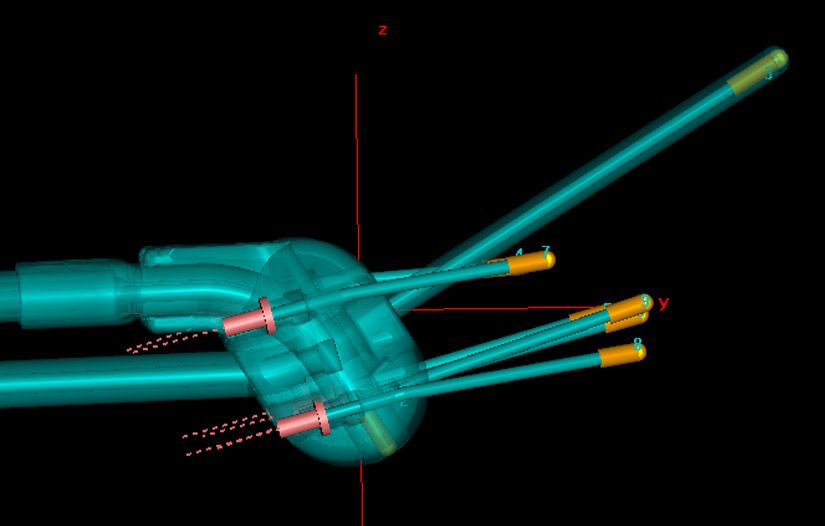
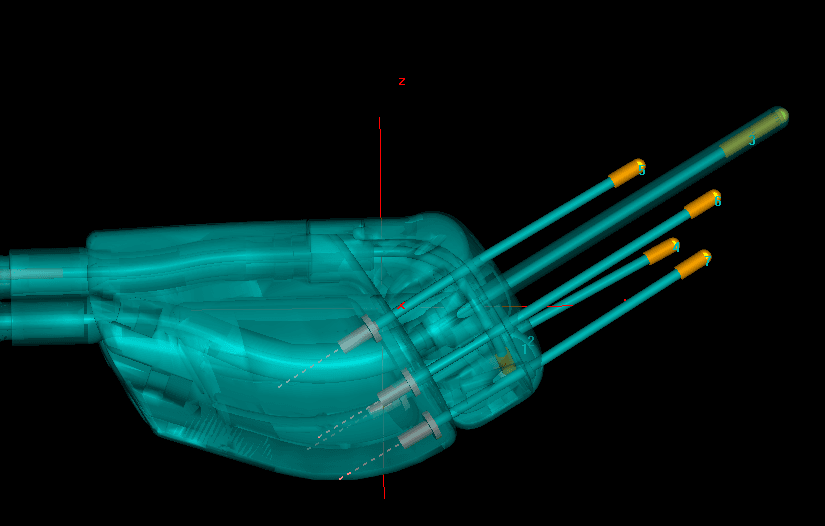
Figure 2. In Geneva (with 13 mm ovoids and 30-dgree IU tube as pictured here), the needles are moving away from the intrauterine tube, while following the line of the tube in Venezia. In only the Geneva 15-degree IU tube will the needles follow the IU tube.
“There will still be a learning curve during clinical use, because the actual needle path depends on the patient’s anatomy and tissue stiffness,” she adds. “Tissue stiffness is also what could force the medial needles to take the road of least resistance toward the uterine intracavitary space, where the intrauterine tube is situated. However, that’s more likely with smaller ovoids in which there is less space for medial needles.”
Interstitial tube
When they encounter a suitable case, the unique Geneva interstitial tube will enable LUMC clinicians to reach cancerous tissue around the vaginal cuff following hysterectomy.
“Some patients who come to our clinic have tumor recurrence on top of the vagina – from primary cervical or endometrial cancers – for which we can use the Geneva interstitial tube.”
“Some patients who come to our clinic have tumor recurrence on top of the vagina – from primary cervical or endometrial cancers – for which we can use the Geneva interstitial tube,” Dr. Velema says. “Depending on the tumor’s location we use different positions for interstitial needles. For central tumors a needle through a channel in the 0 mm intrauterine tube is desirable, which is what Geneva will allow us to do.”
Rectal retractor
For every case moving forward, the LUMC team will use the rectal retractor component of Geneva to spare the rectum.
“In particular the dose to the ICRU rectovaginal reference point will be decreased,” Dr. Velema says. “We are still learning what position is best in what kind of patient/tumor. The retractor has three positions: one reaches under the ovoids, one where it stops just before the ovoids and a third that is in between. The deep position gives more rectal/vaginal sparing, but it can also pull the ovoids away from the cervical ostium in a narrow vagina, making the circumference of the total application larger.”
Acquisition of Flexitron afterloader
When LUMC’s Elekta’s microSelectron afterloader reached End-of-Guaranteed-Support in December 2018, the center acquired the company’s Flexitron® afterloader.
“We changed smoothly and without any doubts to Flexitron,” Dr. Kerkhof says. “The dwell position numbering is much more intuitive compared to microSelectron due to the fixed length of the transfer tubes of 1000 mm and the 1 mm stepsize. In addition, the patient plans and QA plans are appropriately in a separate database as it should be. We also integrated MOSAIQ® Oncology Information System into the workflow to enable patient identification and to enforce patient scheduling and accurate dose registration.”
Overall assessment
In Geneva treatments of LUMC’s first patients, the team’s collective assessment: “Geneva is a straightforward, affordable and easy to assemble applicator to cover a wide range of gynecological tumors, especially due to the 13 mm ovoid size, the decreased offset of the intrauterine tubes, and the interstitial tube for treating recurrent tumors on top of the vagina. Geneva has enlarged our range of possibilities to choose the optimal applicator for each patient, thereby enabling excellent tumor coverage and good sparing of the organs at risk. The overall result is highly individualized cancer care.”
Learn more about Elekta’s Geneva Universal Gynecological Applicator.





