Boosting radiotherapy with brachy
How multi-modality (combined) interventional radiotherapy treatments can improve clinical outcomes
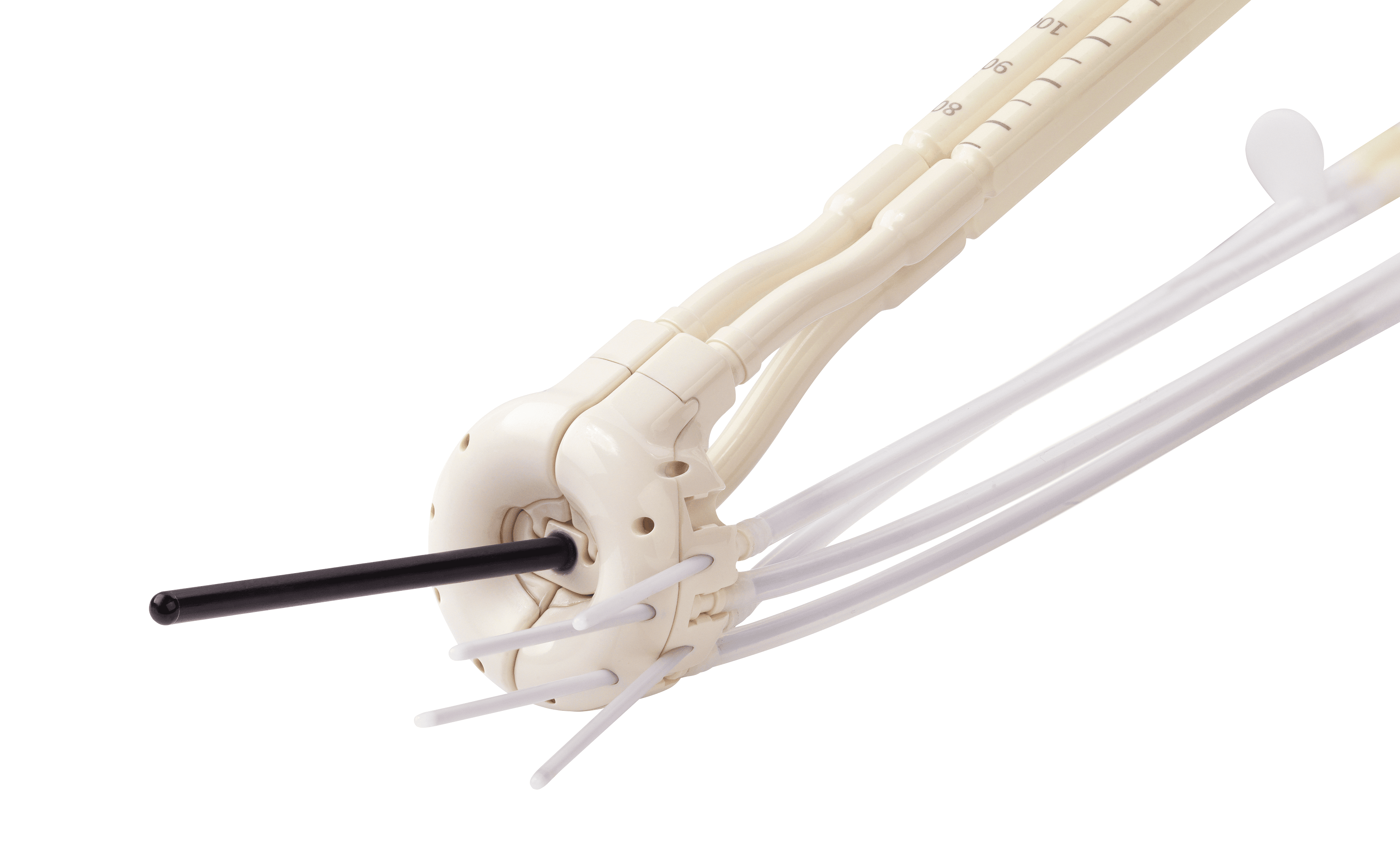
Highly targeted, potent radiation doses delivered with interventional radiotherapy – a brachytherapy (BT) “boost” complementary to external beam radiation therapy (EBRT) – can lead to better local tumor control and higher survival rates for a variety of different cancers, according to Professor György Kovács, a radiation oncologist Gemelli-INTERACTS (Rome, Italy). Prof. Kovács reviewed the rationale and clinical evidence for EBRT plus BT boost during a May 15 webinar hosted by Physics World.

The Elekta-sponsored presentation, titled “Why to boost with interventional radiotherapy?” can viewed here.
A challenge in conventional radiotherapy has been that the homogeneous radiation dose delivered to the tumor often fails to account for regions within the target volume that require a higher dose to be effective. These would include poorly oxygenated areas within a tumor or lesions with a higher stem cell density. Furthermore, often the lower radiation tolerance of target surrounding normal tissue areas do not allow the application of a necessary high dose to the target. Additionally, using high-dose EBRT alone to compensate for this also requires a larger margin of safety around the tumor resulting in not necessary surrounding healthy tissue irradiation.
According to Prof. Kovács, adding a BT boost to EBRT (versus EBRT alone) for local dose escalation has been shown in many studies to improve clinical outcomes for head-and-neck, rectal, anal, breast, cervical and prostate cancers.
Highlights include:
Head-and-neck cancer: The literature shows that a combination of EBRT plus BT can enable a high dose of >90 Gy BED (Biological Equivalent Dose) in the region of the tumor where the highest dose will be necessary. The result comparing BT boost plus EBRT with traditional regimes is a significantly better outcome in cumulative survival compared to IMRT-boosted patients. In addition, using IMRT boost has a considerably higher toxicity due to the dose to larger normal tissue volumes.
Rectal and Anal cancer: EBRT + BT boost provides a superior dose distribution than RapidArc and Cyberknife and results in superior LC and OS.
Breast cancer: The EORTC trials confirmed that local dose escalation by boost radiotherapy reduced the 5-year local recurrence rate by about 50 percent. One such trial involved more than 8,000 women and demonstrated that there is less local recurrence with a tumor bed boost. With BT boost versus EBRT, doses to OARs are also substantially lower.
Cervical cancer: The Vienna group showed that a BT dose escalation from 81 Gy to 90 Gy to the high-risk CTV resulted in 18-20 percent increase in local control. The Budapest group has demonstrated that interstitial BT enables the personalization of the intracavitary dose distribution.
Prostate: Curves comparing 86.4 Gy EBRT beam versus 46 Gy EBRT beam plus 21 Gy HDR brachy boost, showed that there is a significant to combining BT boost and a lower EBRT dose. A UK study – which compared hypofractionated EBRT with lower dose hypofractionated EBRT plus BT boost – showed that the outcome was very good for the BT boost arm. A recent meta-analysis of the published studies stated a Level 1 Group A evidence for better treatment results by using BT boost complementary to EBRT.
Imaging: The use of MRI or CT is a pre-requisite for BT boost planning, although fewer institutions worldwide have ready access to an open MRI, while CT in the BT is quite common. One cervix cancer publication showed that in terms of local control, disease-free survival and overall survival, results for CT-based planning for interstitial dose escalation are very good; there are no major differences in outcomes between CT- and MRI-based planning. In prostate cancer, the expanding role of multiparametric transrectal ultrasound (mpTRUS) in the biological planning of high dose areas was stated.