Australian doctors perform novel therapy for lung cancer

Elekta’s breath-hold system isolates mobile tumor, enabling radiotherapy team to safely treat lesion
Doctors at Nelune Comprehensive Cancer Centre (NCCC, Prince of Wales Hospital, Sydney) combined Elekta treatment solutions to treat a patient with a particularly challenging lung cancer case. In 2016, the 56-year-old patient had received stereotactic body radiation therapy (SBRT) to treat a lung metastasis from metastatic colorectal cancer. Unfortunately, a new lung lesion appeared in 2017 that resisted chemotherapy for the next 12 months, growing from two centimeters to three-and-a-half centimeters.
“The tumor’s size and especially its movement would be problematic if we used our usual free-breathing 4D SBRT technique,” recalls Wenchang Wong, MD, NCCC radiation oncology specialist. “The free-breathing 4D simulation scan showed that the tumor was moving nearly its whole length vertically, causing it to overlap with the treatment field of the first lesion. If we used free-breathing SBRT, the previously treated area would be re-irradiated, which could potentially cause severe side effects.”
Failing an alternative, as he was not a surgical candidate, the patient would have received either no local treatment at all or low-dose palliative radiation therapy. And a fourth round of systemic therapy for this evidently chemo-resistant tumor would likely be ineffective.
Freezing tumor motion with DIBH
Dr. Wong and department physicists ultimately agreed that the best option would be to try respiratory gating with Deep Inspiration Breath-hold (DIBH), a technique commonly used at NCCC to treat liver, pancreatic, mediastinal lymphoma and adrenal cancers, as well as left-sided breast cancer. DIBH radiotherapy freezes tumor motion to maximize the lesion’s distance from surrounding normal tissues.
In this patient’s case, the NCCC team surmised that DIBH could sufficiently separate the new lesion from the previously treated tumor field.

“Using DIBH to treat lung cancer with SBRT is a radical departure from our 4D ITV-based approach – we’ve never done it for lung cancer before, this would be a first,” says NCCC radiation therapist David Nguyen.
NCCC clinicians had a range of Elekta technology on hand to facilitate the patient’s DIBH treatment, most notably the company’s Active Breathing Coordinator™ which helps regulate and monitor the patient’s breathing cycle by measuring the patient’s inspiration and expiration volumes. Active Breathing Coordinator is linked to NCCC’s Versa HD™ linear accelerator through Elekta’s Response gating interface, enabling the delivery of automated, gated breath-hold treatments. Response activates the treatment beam when patients hold their breath and instantly, automatically shuts off radiation when patients resume free-breathing.
The patient was coached to hold his breath for 30-second intervals for treatment and simulation. The latter consisted of two CT scans – a DIBH scan and a free-breathing scan – to evaluate the degree to which DIBH would separate the lesion treated earlier from the new tumor.
“The DIBH scan showed that on deep inspiration the edges of the tumors were three centimeters apart, which would be a sufficient buffer zone to avoid irradiating the previous field.”
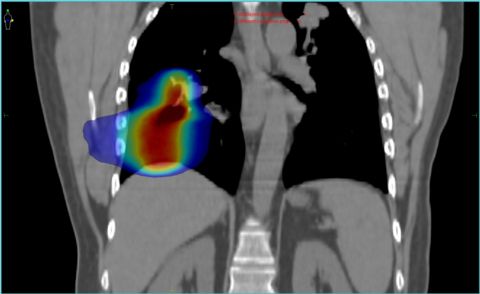
“The DIBH scan showed that on deep inspiration the edges of the tumors were three centimeters apart, which would be a sufficient buffer zone to avoid irradiating the previous field,” Dr. Wong notes.
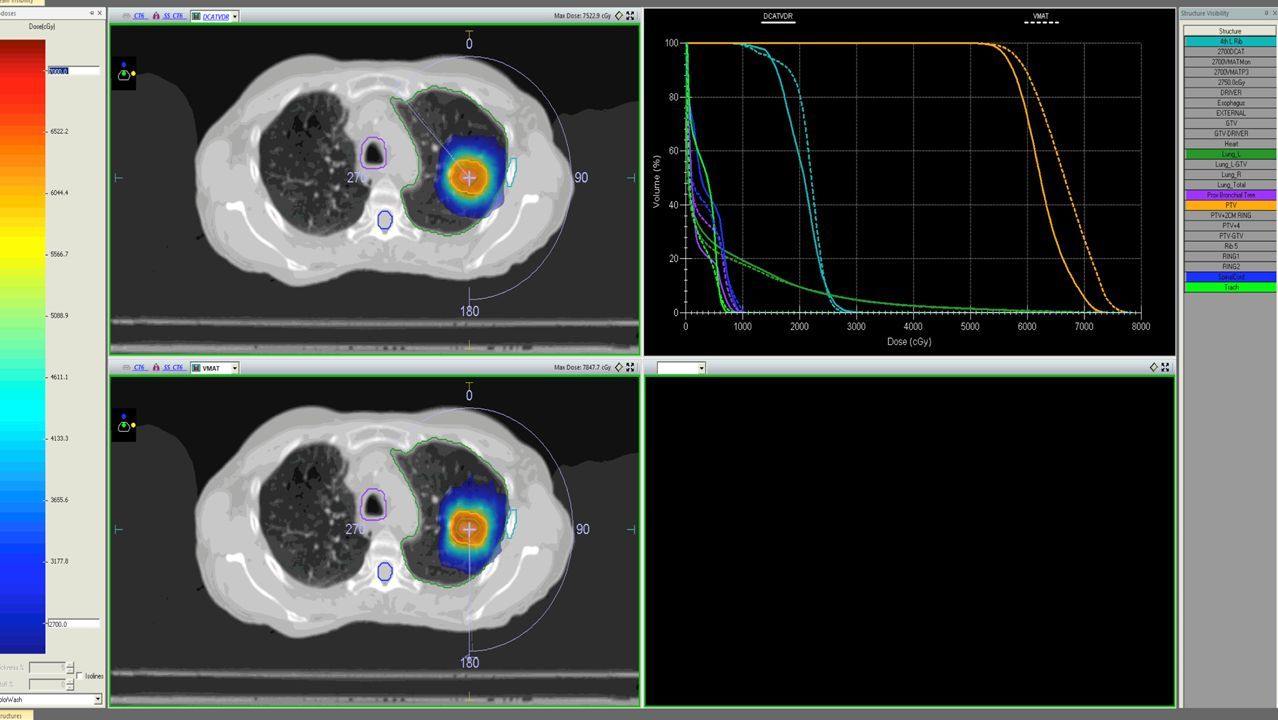
Clinicians used the DIBH scan to plan the treatment using Elekta’s Monaco® treatment planning system.
“We routinely plan our SBRT patients on Monaco mainly because it uses the Monte Carlo algorithm,” Nguyen says. “The algorithm accurately calculates the dose under conditions of lateral electronic disequilibrium typically found in lung SBRT treatments.”
The SBRT treatment was prescribed at a potent 12 Gy per fraction over four fractions every other day for a total dose of 48 Gy.
High Dose Rate mode slashes SBRT beam delivery time
High dose per fraction SBRT beams like the ones used in this lung cancer patient’s case can take some time to deliver, so the NCCC team decided to use their the Versa HD High Dose Rate (flattening filter-free, FFF) mode, which would reduce the beam delivery time considerably.
“We calculated the beam delivery time for High Dose Rate mode was about nine minutes, compared to around 15 minutes without High Dose Rate mode,” Dr. Wong says.
According to Daniel Au, NCCC radiation therapist and research coordinator, reducing beam delivery time in SBRT not only increases patient comfort, but it also contributes to patient safety.
“Using High Dose Rate mode can increase patient comfort and compliance in completing each treatment session safely and without interruptions.”
“The time to deliver the planned dose in SBRT can be especially long in cases that involve pulmonary gating as in Active Breathing Coordinator, which can lead to intrafraction motion by the patient,” he observes. “Using High Dose Rate mode can increase patient comfort and compliance in completing each treatment session safely and without interruptions.”
The patient’s four fractions were delivered in an average of just eight minutes per fraction.
Precision and safety were also enhanced in this patient’s case with the use of Elekta’s HexaPOD™ evo RT System, a robotic patient positioning system for SBRT that enables six degrees of sub-millimeter patient positioning freedom (x, y, z, roll, pitch, yaw)
“HexaPOD was critical in ensuring that tumor targeting during set up was accurate because we were giving such a high dose per fraction,” Daniel adds.
A new treatment option for lung cancer patients
Three months after treatment the patient had his first follow-up scan – and the news was good.
“The lesion had decreased in size by a centimeter – from 3.2 centimeters to two centimeters,” Dr. Wong reports.
The prevalence of patients who present at NCCC with the characteristics of their first DIBH/Active Breathing Coordinator/respiratory gated lung cancer patient is not high, but Dr. Wong just ran across one at press time.
“Coincidentally, we just simulated another such patient this morning,” he relates. “She has two lung lesions from metastatic colon cancer for which we were calculating the separation. The vertical separation is just a centimeter, but the anterior-posterior distance was five centimeters. The bottom lesion moved a lot more than the top lesion. We decided to use DIBH for her today in order to get the greatest separation between the two tumors so that when we put the beams on her we will be able to minimize that overlap you get in the free-breathing 4D technique.”
For the subset of patients who either have a new lung lesion near a previously irradiated tumor and for those whose amplitude of tumor motion puts two lesions too close together, DIBH with Active Breathing Coordinator and High Dose rate (FFF) mode presents a desirable alternative to either a poor option or no treatment.
“The combination of these Elekta technologies – systems that we use every day in our clinic – provides an elegant solution for these lung cancer patients.”



The Nelune Comprehensive Cancer Centre is bright and serene for patients and staff, providing coordinated inpatient, outpatient and ambulatory care to patients. The Centre is a major teaching hospital, training oncologists, radiation therapists, physicists and nurses.
“The combination of these Elekta technologies – systems that we use every day in our clinic – provides an elegant solution for these lung cancer patients who present tumor motion characteristics that would otherwise make them ineligible for conventional free-breathing SBRT,” Dr. Wong says.