Australian cervical cancer patients benefit from clinic’s latest Elekta GYN applicator

The Geneva Universal Gynecological Applicator is new “go-to” solution at Olivia Newton-John Cancer Wellness and Research Centre

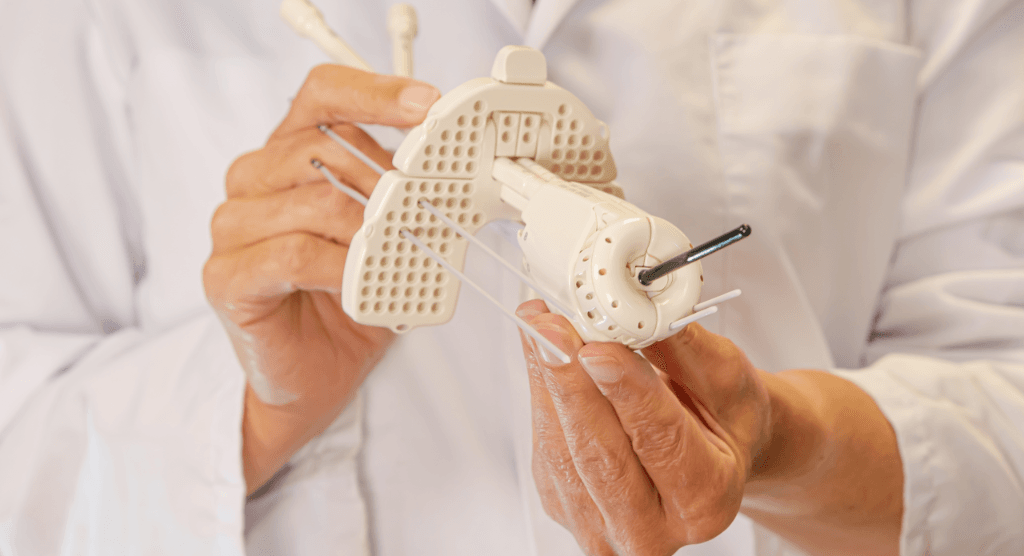
Olivia Newton-John Cancer Wellness and Research Centre (ONJ, Melbourne, Victoria) clinicians began using their new Geneva™ Universal Gynecological Applicator in October 2020 and in a very short time it became the clinic’s preferred applicator for patients with cervical cancer – accounting for three out of every four treatments. According to ONJ radiation oncologist Dr. Carminia Lapuz, Geneva is capable of treating a wide range of cervical cancer cases, assembles easily, provides excellent coverage of the uterine fundus and is less expensive than other hybrid applicators.
At the establishment of ONJ’s MRI adaptive brachytherapy program in July 2016, clinicians were using the Utrecht hybrid applicator and the multi-channel vaginal cylinder (MCVC) and in time added a standard CT/MRI applicator. In 2018, ONJ began using Elekta’s Venezia™ Advanced Gynecological Applicator.
“Last year, we acquired the Geneva applicator on the strength of several aspects of the device in comparison with our existing applicators.”
“Venezia quickly became our applicator of choice due to its ease of use and fantastic dosimetry, and so we decommissioned the Utrecht applicators,” Dr. Lapuz says. “Last year, we acquired the Geneva applicator on the strength of several aspects of the device in comparison with our existing applicators.”
According to Dr. Lapuz – apart from Geneva’s economical price – these include:
- Shorter offset (i.e., dead space) of 0.8 cm in the Geneva intrauterine tubes (IU), versus the longer 1.2 cm offset of the Venezia IU tubes. Also, the Geneva has an 8 cm IU length, versus the longest 7 cm IU tube of Venezia. Both of these features provide better coverage of the uterine fundus.
- The interstitial lunar ovoids of Venezia are too large for smaller pelvic anatomies; clinicians would have to use small standard ovoids or small MCVC, resulting in limited coverage of bulkier tumors without the interstitial catheters. With Geneva there is a small (13 mm) interstitial ovoid option.
- In the post-hysterectomy setting in which the cervical stump is treated, Venezia – with the 0 cm tandem – provides a simple interstitial option, but ONJ clinicians found the dosimetry was somewhat colder centrally than desired. Geneva offers an interstitial IU tube – essentially a 0 mm tandem with an interstitial catheter – allowing the use of an interstitial catheter where a tandem normally would be employed.
In August 2020, ONJ acquired a Geneva kit with five ovoid sizes [mm]: 13, 15, 20, 25, 30 and IU lengths [mm] of: 0, 30, 40, 50, 60, 70, 80 and the interstitial tube.

“The 30-degree tandem is the angle we determined we would most commonly use in our department and we also bought the 15-degree tandem to provide the option of having the ovoid interstitial catheters parallel to the IU tube,” she notes. “This is useful if we need to cover anteriorly with the anterior interstitial catheters.”
The center commissioned Geneva in September 2020 (see sidebar ONJ Geneva commissioning) and on October 5, 2020, the brachytherapy team treated their first patient using the applicator (see sidebar Geneva debuts at ONJ). Today, ONJ averages about eight Geneva insertions each month.
Reflections on Geneva
By May 2021, after having used Geneva to treat 10 cervical cancer patients, Dr. Lapuz, together with senior brachytherapist Sylvia Hanna and deputy charge brachytherapist Nicola Oliver, have had time to evaluate the features and characteristics of the applicator.
The IU tube’s shorter offset (versus Venezia) has helped the team improve dosimetry for the entire uterus, according to Oliver.
“The smaller dead space of Geneva means we can get more dose to the fundus in comparison to Venezia, so we have definitely noticed a massive benefit in dosimetry to the fundus,” she says.
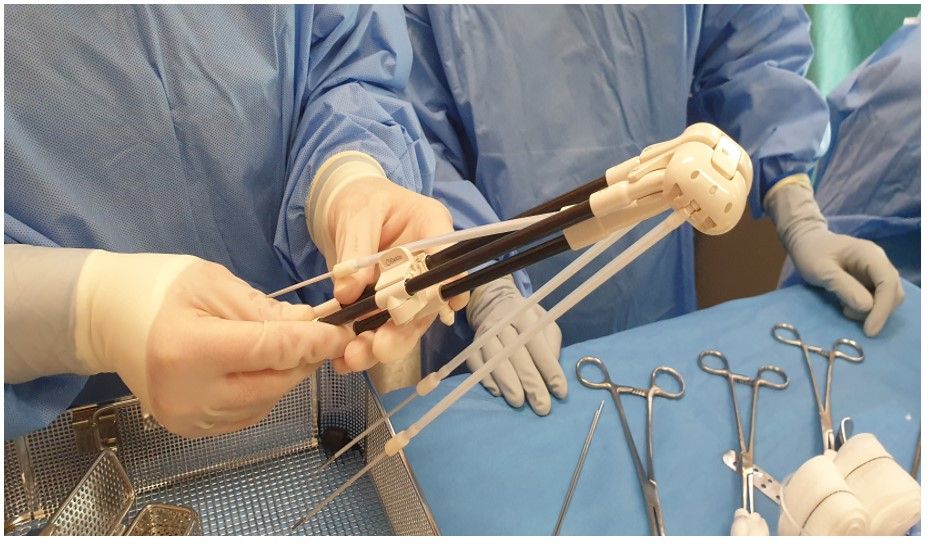
“Geneva assembly requires no screws – it takes literally four clicks and it’s assembled.”

Oliver and Hanna are among ONJ’s radiation therapists who are tasked with assembling GYN applicators in-theatre in preparation for cases.
“It’s fair to say that Geneva is the easiest applicator to put together, especially if you compare it to the Utrecht applicator, which required several tiny screws,” Hanna observes. “With gloves on it was easy to drop a screw, which would often bounce off the sterile table to the floor. Geneva assembly requires no screws – it takes literally four clicks and it’s assembled.”
Hanna and Oliver also perform planning for Geneva on the Oncentra® Brachy treatment planning system.
“It’s very similar to planning with the standard CT/MR Standard applicator,” Hanna says. “The applicator modeling on the system is great and accurate. Our processes haven’t changed with Geneva in terms of reconstruction and planning.”
“Moving from our Venezia, our former ‘go-to’ applicator, to Geneva was very straightforward,” Oliver adds. “It was not a massive learning curve from a planning standpoint.”
For optimization during planning, Dr. Lapuz comments that the ring-and-tandem design of Venezia helps shape the dose around OAR, especially the rectum, without compromising dose elsewhere.
“The Geneva dosimetry is similar to the standard applicator with the square shape of the ovoids, and shaping around the rectum is limited,” she says. “We also found the vaginal doses to be lower with Venezia compared with Geneva or the standard applicator. With the MCVC, it’s difficult to achieve a good dose at the base of the cervix, as you only have the IU contributing to the dose. Venezia, with its oblique needles, allows excellent coverage of very bulky or pelvic sidewall tumors, but Geneva – with the interstitial catheters – can provide good coverage of stage 2B disease. If the patient has mid- to lower vaginal disease you can’t use Venezia or Geneva for these cases.”
To persuade a center to explore the feasibility of Geneva for their clinic, both Oliver and Hanna point to a combination of advantages in a single applicator.
“From our point of view, Geneva covers a lot of our needs in brachytherapy.”
“It’s easy to assemble, insert and remove,” Hanna says. “Plus, it’s very cost-effective and you’ve got the great option of interstitial needles, the interstitial IU and the shorter offset. From our point of view, Geneva covers a lot of our needs in brachytherapy.”
“There’s a wide variety of ovoid sizes, especially the 13 mm ovoid, which we’ve actually used a couple of times,” Oliver adds. “There are very good options for varied anatomies.”
*Photo taken before mask-wearing regulations were introduced.
Geneva debuts at ONJ
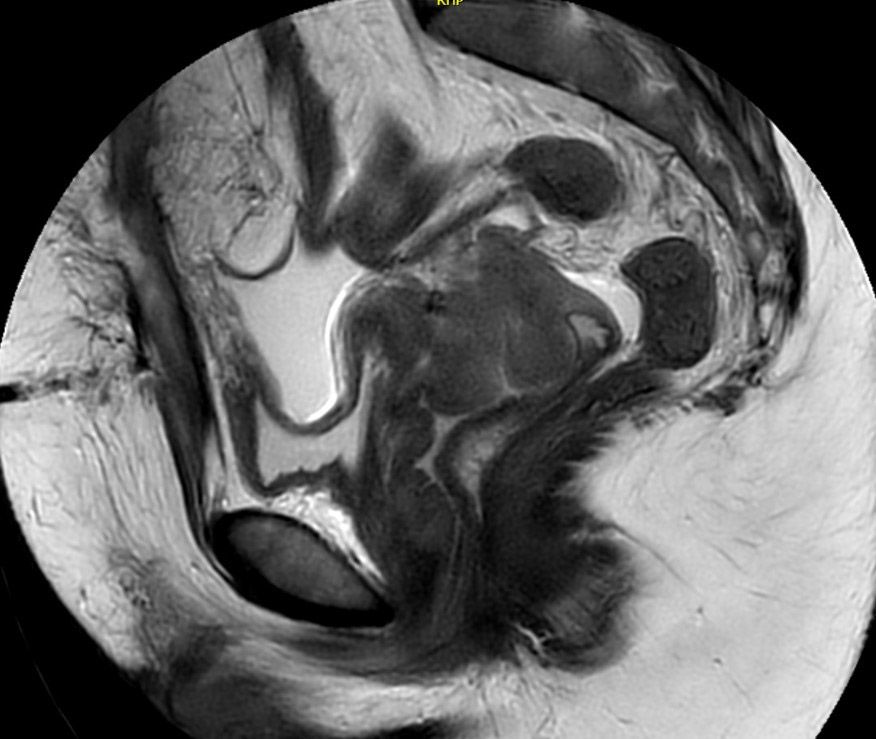
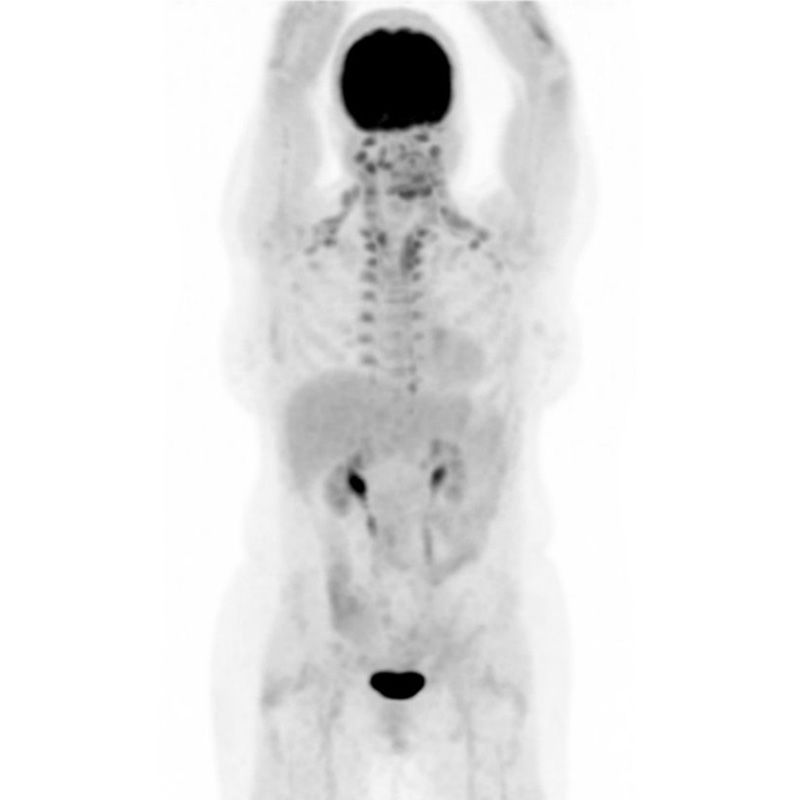
ONJ’s first Geneva case, a 43-year-old with a history of subtotal hysterectomy, presented with PV bleeding and was found to have a cervical squamous cell carcinoma on biopsy (Figure 1). A PET scan also showed pelvic and retroperitoneal nodes, indicating stage 3C2 disease (Figure 2). She was treated with a course of EBRT with weekly cisplatin followed by brachytherapy.
“Because of the previous hysterectomy, Geneva was a great applicator choice for her as the interstitial IU tube option would allow good central tumor dose and provide a simpler interstitial option for us,” Dr. Lapuz observes. (Figure 3)

Insertion of the interstitial tube required several attempts to optimize position; the metal obturators inside the interstitial catheters caused substantial reverberation and artifact on ultrasound, which made visualizing interstitial tube placement somewhat challenging.
“First, we tried pre-plunging before insertion to 2 cm depth and, after dilating the cervical os, inserted like we would an IU tandem,” she explains. “We found at MRI, however, that the tube sat posteriorly, which hadn’t been obvious on ultrasound and also that the tube was more bent than desired.”
For the next fraction, the brachytherapy team tried positioning the tandem over the os and plunging 2 cm, but the catheter still sat too posteriorly. Consequently, for the final fraction, they tried a combination and pre-plunged 1 cm, then positioned in the os before plunging the remaining 1 cm.
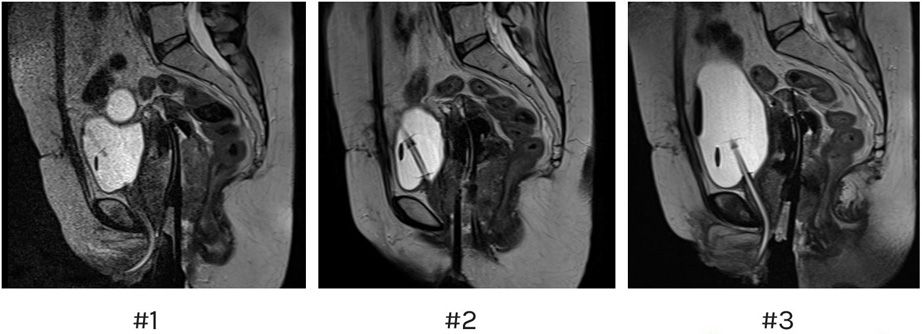
“This again was too posterior, so for this first patient the best position we found was achieved by pre-plunging to 2 cm and inserting like a tandem,” Dr. Lapuz says. “We also decided to use the C and D catheters on both ovoids to achieve tumor coverage. On ultrasound at fraction 1, due to the perceived proximity to bowel, the 1C and 2C catheters were only inserted to 1 cm, while the 1D and 2D catheters were inserted to 2 cm. However, the MRI showed that there was room to insert the C catheters further to 2 cm for better tumor coverage, which we did on subsequent fractions.”
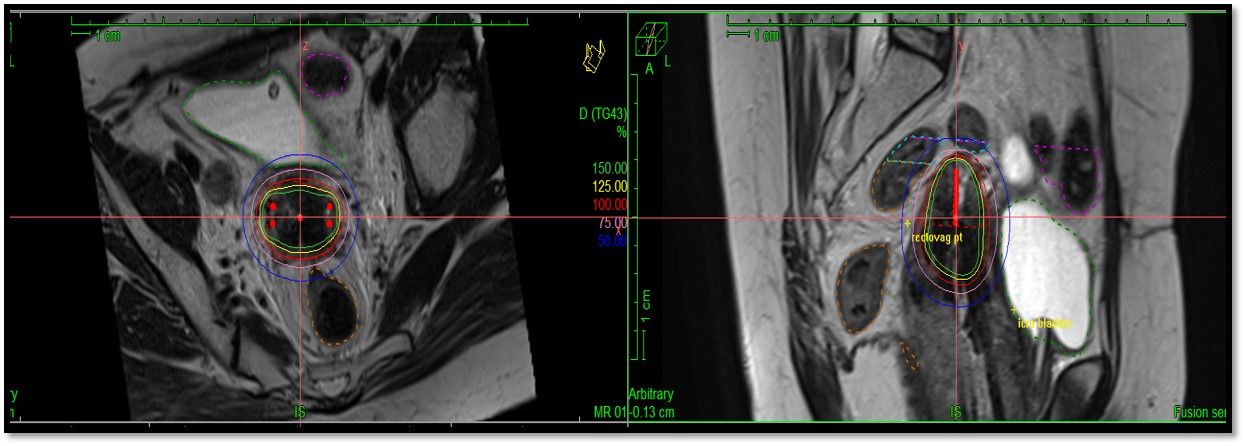
For optimization during planning, ONJ radiation therapists treated the interstitial tube like an intrauterine tandem and loaded the dwell positions more heavily compared with the ovoid catheters. Coverage was improved for subsequent fractions after inserting the C catheters further to 2 cm and the team was able to deliver over 80 Gy EQD2 to the HRCTV. (Figure 4)
“Due to the Covid-19 lockdown in Melbourne at the time, we had to reduce the number of brachytherapy fractions from four to three to minimize patient visits, so we didn’t have that extra fraction to improve total HRCTV dose,” she says. “Another limiting factor for this case was that sigmoid and rectum were very close to the HRCTV. Our policy is to minimize 75 percent isodose crossing these structures, particularly with the three-fraction regimen, which limited the total dose to the HRCTV.
The three-month post-treatment PET scan (Figure 5) shows that the patient had a complete metabolic response.
ONJ Geneva commissioning
The Geneva applicator was comprehensively evaluated by the Austin Health radiation oncology medical physics (ROMP) team prior to clinical use. Senior radiation oncology medical physicists Tom Kupfer and Hema Vaithianathan report on Geneva commissioning:
“The applicator parts that ONJ uses can be assembled into 65 configurations that allow treatment of a wide range of anatomies and clinical situations. Using CT, the applicator’s dimensions were independently verified on-site. CT images of the assembled applicator matched the model provided with the Oncentra Applicator Library. The dwell positions of the brachytherapy source within the intrauterine and ovoid tubes were determined using autoradiographs. All dimensions and dwell positions were found to agree with vendor specifications within the tolerances recommended by the Australian College of Physical Scientists & Engineers in Medicine.
“Provision of the interstitial tube benefits some of our patients, with certain clinical conditions, where an intrauterine tube cannot be used. The interstitial tube and ovoids can accommodate hollow plastic needles that allow source placement in target anatomy where it would otherwise not be possible. Determining the insertion depth of plastic needles from MR images is difficult compared to CT images. As many of our patients are planned based on MRI, there is a need to validate geometry with this modality. The team, therefore, developed an additional method to determine insertion depths, by taking into consideration the total length of the needles and the dimensions of the precisely manufactured applicator.
“Radiation oncologists, radiation therapists and ROMP jointly established rigorous quality documentation to define safe clinical workflows. Bringing this innovative technology into a busy brachytherapy service for the benefit of patients at Austin Health was a multi-disciplinary effort.”