Australia center boosts brain SRS capacity with Gamma Knife

Peter MacCallum Cancer Centre’s radiotherapy department covers the full spectrum of intracranial SRS indications
With growing demand for both its SABR (stereotactic ablative radiotherapy) and SRS (stereotactic radiosurgery) services, Peter MacCallum Cancer Centre (Peter Mac) moved to boost capacity to meet the rising number of patients needing precision radiation therapy. The 2020 acquisition of Leksell Gamma Knife® Icon™ enabled its Department of Radiation Oncology to shift 85 to 90 percent of its brain caseload, half of which comprises metastases, away from SRS delivered on a stereotactic linear accelerator to a dedicated intracranial SRS system. During the last 18 months of Icon use, Peter Mac physicians have not only unburdened their linear accelerators, but they also have diversified their case mix to include the treatment of AVMs, trigeminal neuralgia, pituitary adenoma, schwannoma and meningioma. With access to Gamma Knife Icon as well as linacs, Peter Mac is fully equipped to treat virtually any intracranial indication, and offers a more personalized approach to each patient’s treatment.

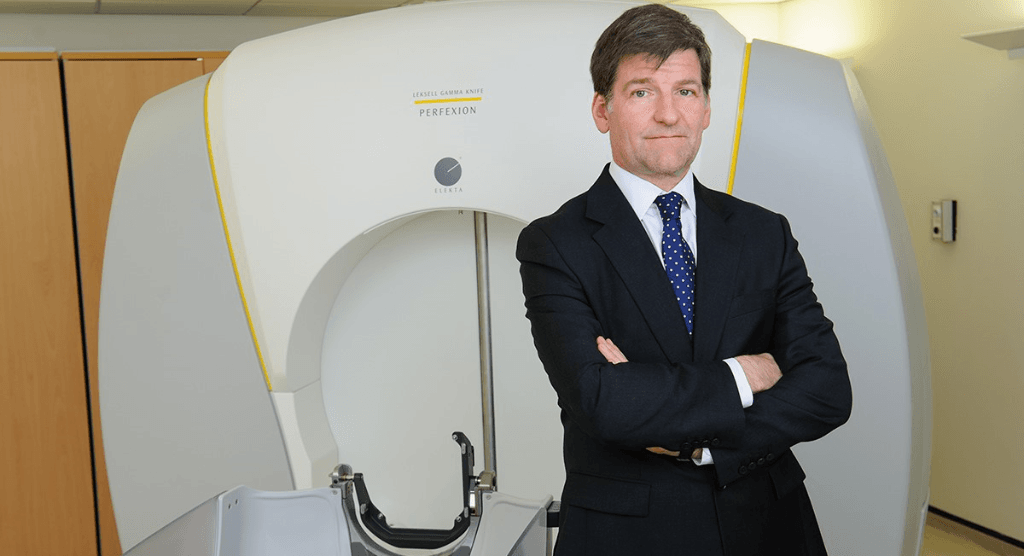
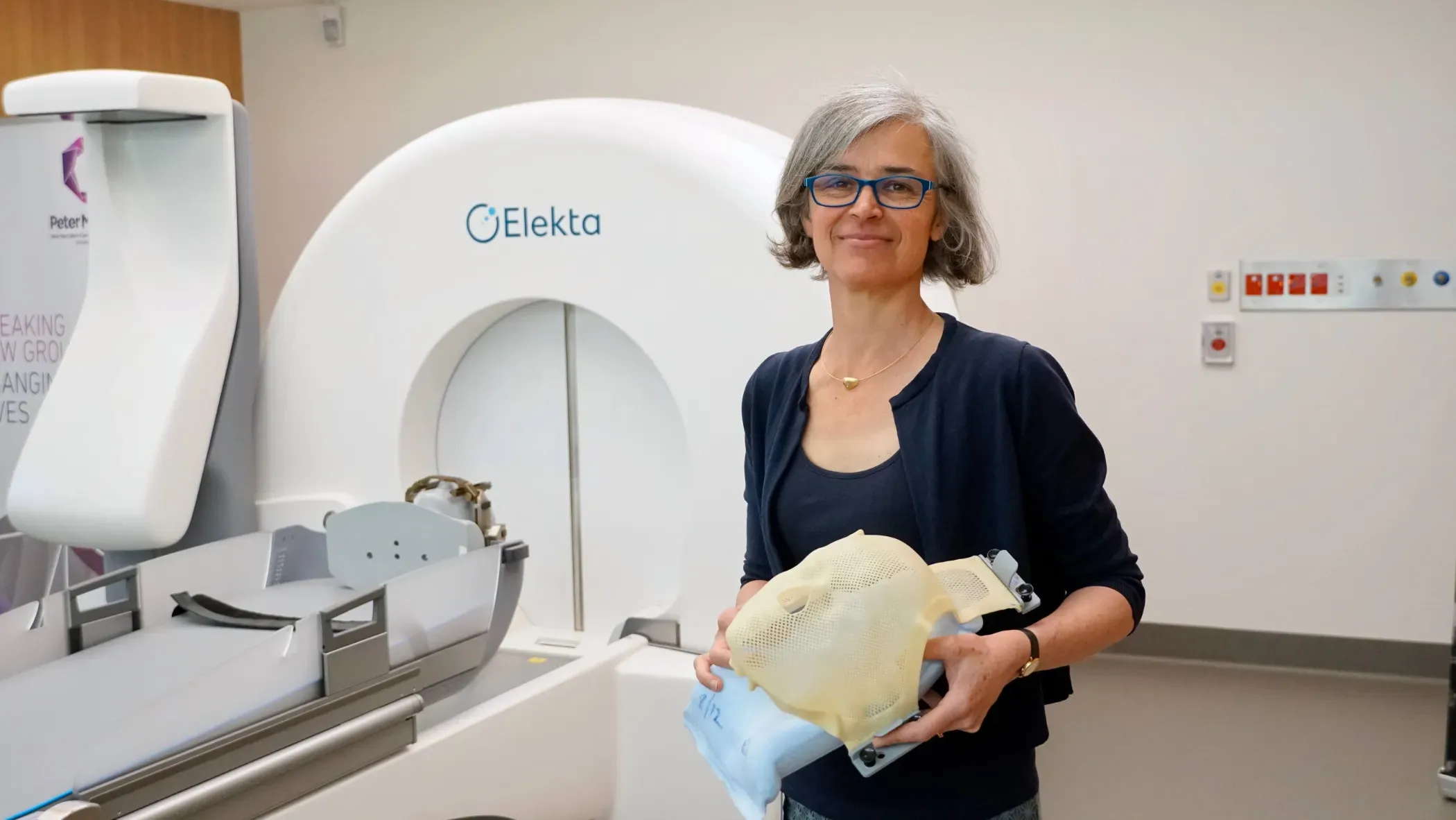
“When we first introduced linac-based SRS, Icon hadn’t been launched yet and we wanted something that wasn’t purely frame-based,” says radiation oncologist Claire Phillips, MD, Deputy Director of the Department of Radiation Oncology at Peter Mac, and administrator of the Victorian Gamma Knife Service at Peter Mac. “Icon introduced frameless, mask-based radiosurgery, which completely changed the utility of Gamma Knife technology, and with its dosimetric and efficiency advantages over linac SRS – especially for mets – acquiring Icon was a ‘no-brainer.’”
Starting up during worldwide lockdown
The delivery of the Icon to Peter Mac in October 2020 was complicated by the spread of Covid-19 across the world, forcing severe restrictions and lockdowns in Victoria. Icon staff training and installation were challenges as in-person visits were prohibited.
Fortunately, University of Pittsburgh Medical Center and Cleveland Clinic had developed online programs in which Dr. Phillips, Neda Haghighi, MD (NeuroOncology Lead radiation oncologist), neurosurgeon Dr. Andrew Davidson, physicists and RTTs participated. In addition, Gamma Knife veterans Dheerendra Prasad, MD and Ian Paddick assisted remotely before and after go-live. From the start, Peter Mac has enjoyed the online and in-person assistance of professionals at Brisbane’s Princess Alexandria Hospital, which has operated an Icon system since 2018.
“Training and installation went remarkably smoothly,” Dr. Phillips recalls. “The original goal had been November 2020, but lockdowns in Victoria slowed things down. We started treating patients on February 1, 2021. We had the advantage of already being quite comfortable performing linac SRS, so we were able to hit the ground running.”
“We had expected huge delays, but the training and implementation process went unbelievably well.”
Dr. Haghighi, clinical lead of Peter Mac’s Gamma Knife service, adds: “We had expected huge delays, but the training and implementation process went unbelievably well. It took six or seven months from the time we purchased Icon to when it was in the department, then a few more months for commissioning.”
The first patient Peter Mac clinicians treated with Icon had a meningioma and this was quickly followed by a variety of classic Gamma Knife indications, including pituitary adenoma, trigeminal neuralgia, acoustic schwannoma and metastases. The first AVM treatments would follow a few weeks later.
An efficient platform for metastases
For years, Peter Mac clinicians had been using their linac to deliver SRS to one or more brain metastases, but the number of mets and their size often presented complications.
“We were restricted in what we could do on the linac, because once you get more than about four lesions, planning becomes burdensome,” Dr. Phillips notes. “In addition, treating very tiny lesions was problematic from an accuracy point of view – we thought the probability of error was too high, so we would just watch those lesions and have another look in a few months or possibly opt to deliver WBRT.
“Planning and treating more than four mets on Icon is easy and straightforward.”

“Planning and treating more than four mets on Icon is easy and straightforward,” she adds. “And access to the system has been better. For example, for patients who need to start their systemic therapy quickly, we can get them planned and treated so rapidly with Icon that we’re doing a lot more of that as well.”
Icon also has enabled Peter Mac to recruit mets patients for clinical trials, Dr. Haghighi says.
“As an academic hospital we have many active brain mets trials,” she observes. “With Icon, we treat everyone without hesitation, regardless of the number of mets or how small they are.”
Another aspect boosting the center’s brain mets workload is the convenient Icon workflow.
“We treat a lot of patients from rural areas far from the hospital,” Dr. Haghighi says. “Before Icon, these individuals had to come to the hospital a few times before treatment. Now we see them on Telehealth. They come to the center for imaging, simulation and treatment on the same day. It’s just one trip for them.”
Immobilization options
While a single treatment session is practical for patients with one or a few (i.e., 3-4) lesions, patients with several mets typically receive fractionated radiosurgery.
“This is where using mask immobilization has been useful,” Dr. Phillips says. “Patients with many mets or who are facing long treatment delivery times might have, for example, five lesions treated one day and three lesions the next to make it more manageable for the patient, rather than having them lie on the couch for a long time.”
Dr. Haghighi adds that clinicians also employ the mask for patients with large, benign skull base tumors requiring fractionation. The G-frame or Leksell® Vantage™ Stereotactic System is utilized for patients with benign tumors and single-session treatments that require rigid fixation.
“Frame-based radiosurgery always provides the best immobilization for when accuracy is crucial, for instance, when a benign tumor is right up against the optic nerve, or in cases in which you want to reduce the risk of long-term side effects, for instance, patients with a long life expectancy,” she explains. “We also use the frame for functional indications like trigeminal neuralgia and for vascular disorders, such as AVMs, as well as schwannomas and complex pituitary adenomas.”
Planning at Lightning speed
For the first six months of Icon use, Peter Mac staff performed manual forward planning with Leksell GammaPlan®, something that Drs. Haghighi and Phillips viewed as a benefit as new users of Gamma Knife technology.
“I must admit I think that was great,” Dr. Phillips says. “Learning how to plan is critical. The automation in the Lightning treatment plan optimizer [LGP v.11.3.1] nearly eliminates the need to develop that skill. That said, Lightning is a substantial improvement – the speed is incredible.”
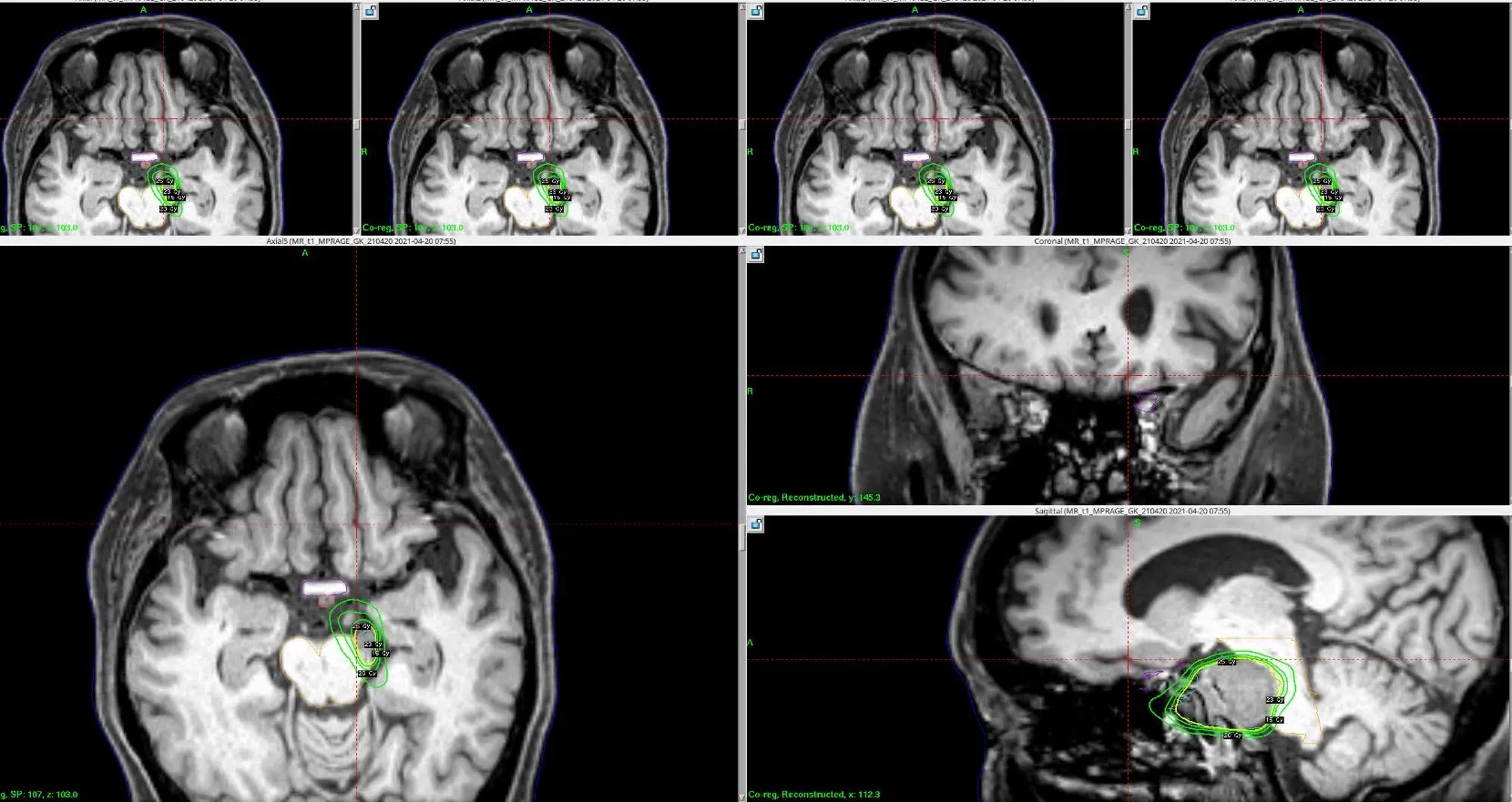
She explains that Gamma Knife Lightning is used extensively for patients with multiple mets, the optimizer providing a “first shot,” followed by manual adjustments. Dr. Phillips relates a “very tricky case” in the initial training days with Lightning.
“That first week with Dr. Prasad we had a case with a bit of residual pituitary disease that was right up against the optic chiasm,” Dr Haghighi recalls. “We spent ages trying to reduce the dose to the optic chiasm. Dr. Prasad used Lightning and it took about 30 seconds to create a better plan.”
“Lightning sometimes takes literally 10 seconds to develop a plan.”
“I wish we would have had a longer time with manual planning for us to get really good at it, but Lightning has made life so much easier. As its name suggests, the optimizer is as fast as lightning,” she observes. “Lightning sometimes takes literally 10 seconds to develop a plan. About 60 percent of the time for benign cases, Lightning will yield a plan rapidly and I then manually adjust it. It has been particularly useful for multiple brain mets cases.
“For most of the skull base cases and complex indications it has helped us create incredible plans that we weren’t able to do before.” (Figure 1)
Preoperative Gamma Knife SRS for brain mets
In 2018, Dr. Haghighi’s team began using their linac to perform preoperative (versus postoperative) SRS for brain mets and published the results of their study in April 2022.1
The current standard of care is for patients to receive postoperative SRS of the surgical cavity to address the high risk of recurrence.
“Postoperative SRS is problematic due to difficulties in targeting large cavities,” she explains. “Also, if the met is operated on before SRS, there’s a reasonably high risk of causing leptomeningeal disease, a usually fatal illness. However, if you deliver SRS before surgery, the theory is you can sterilize the tumor cells, potentially reducing the likelihood of leptomeningeal disease.
“Additionally, with preoperative SRS, targeting a small met instead of a large cavity enables you to reduce the risk of radionecrosis,” Dr. Haghighi continues. It’s hard to convince surgeons to let us do radiation first, but once more results from randomized studies are available that should change. I think preoperative SRS will probably become the standard of care in the next five years, and this will be an excellent indication for Icon and increase our Gamma Knife caseload.”
2022 and beyond
Since Peter Mac clinicians began using Icon, more than 400 patients (> 700 sessions) have received Gamma Knife radiosurgery for a variety of indications. These include AVMs, which have seen an increase in patient numbers to one or two each week.
“We recently started our GK AVM program and referrals are coming in rather fast now,” Dr. Haghighi notes. “We’re also working to expand frame-based treatments for benign lesions. My plan for next year is to do four or more frame-based treatments each week. In addition, we plan to start treating functional disorders other than trigeminal neuralgia, such as essential tremor and Parkinson’s disease.*”
According to Dr. Phillips, the efficiency of SRS with Icon cannot be overstated.
"A patient can be referred, have their MRI, CT, mask and cone beam CT, and by the afternoon we’ve treated six brain mets – we can’t do that on the linac.
"Patients with brain mets have many things happening in their lives, so making one of these aspects as simple and efficient as possible is invaluable,” she adds. “Icon has enhanced our ability to care for patients across a wide range of diseases,” she adds. “It has been a really valuable experience. Everyone here feels very proud of what we’ve achieved.”
Dr. Haghighi concurs regarding the versatility and effectiveness of Icon.
“…in my mind no other stereotactic solution can attain the conformity and gradients we can attain with Gamma Knife.”
“The efficacy of Icon is superior to other SRS platforms and once the team has built enough experience and confidence, the system is very simple to use,” she says. “Icon is truly a multipurpose system that enables us to treat malignant, benign, vascular and functional disorders. The workflow is exceptional in terms of patient comfort and in my mind no other stereotactic solution can attain the conformity and gradients we can attain with Gamma Knife. Our overall experience has only been positive.”
Learn more about radiosurgery with Leksell Gamma Knife.
References
- Udovicich C, Ng SP, Tange D, Bailey N, Haghighi N. From Postoperative to Preoperative: A Case Series of Hypofractionated and Single-Fraction Neoadjuvant Stereotactic Radiosurgery for Brain Metastases. Oper Neurosurg (Hagerstown). 2022 Apr 1;22(4):208-214. doi: 10.1227/ONS.0000000000000101. PMID: 35234410.
*Gamma Knife radiosurgery is not cleared for use for the treatment of Parkinson’s disease.
LARLGK230103