Aiming for near-zero risk of virus spread in the radiotherapy environment
Chinese hospital at Covid-19 epicenter develops all-inclusive guidelines to protect cancer patients and RT staff
Radiotherapy leaders at Tongji Hospital in Wuhan, China – Covid-19’s putative city of origin – understand the risk that their vulnerable patients and radiotherapy staff face every day from the deadly virus. Determined to do something to reduce the risk of spreading coronavirus, a Tongji Hospital team produced a comprehensive set of procedures titled “Detailed Implementing Rules [DIR] for Radiation Therapy Under Coronavirus Disease (Covid-19) Outbreak.”
The guidelines – delivered mostly electronically to all department employees – include training and education on epidemic prevention knowledge, prevention and protection of work staff and patients, treatment process optimization, site disinfection and isolation, use and management of protection articles and emergency management.
“Compared with people in the general population, cancer patients have a higher risk of becoming infected due to their weaker immune system,” says DIR co-contributor Professor Hu Guangyuan, MD, PhD. “Once patients are infected, it not only delays their cancer treatment, but also increases the severity of their cancer, leading to a higher risk of death.”
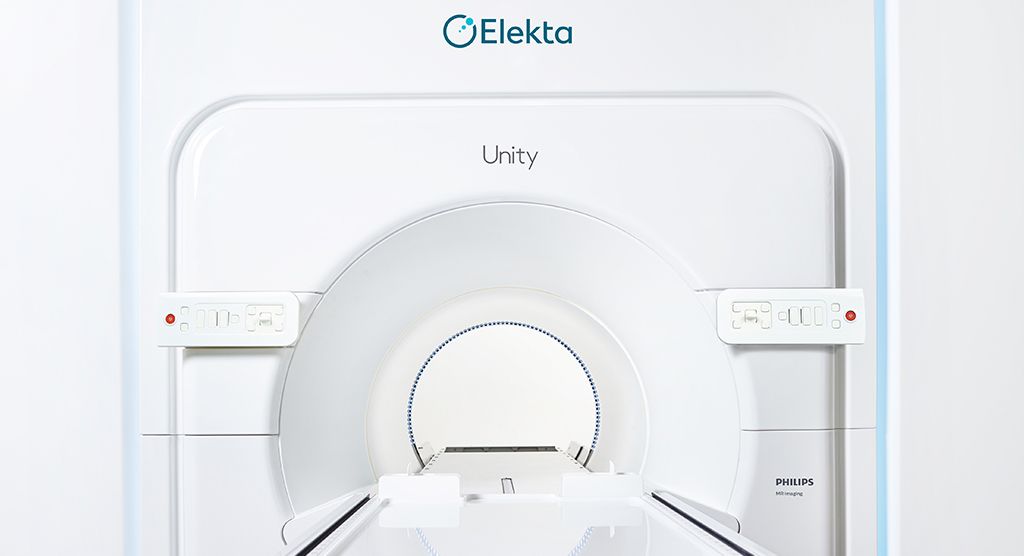
He adds that the radiotherapy environment presents special challenges in preventing the spread of pathogens; the radiotherapy shelter is a closed-in space without windows and is a high-traffic area during clinic hours.
Social distancing
The DIR’s recommendations for patients include alerting them to the risk of cross-infection and signing of informed consent, in addition to avoiding family accompaniment unless necessary or gatherings of family members at the RT center. The RT center should have just one entrance for patient entry and departure and subsequent patients can enter only after the previous patient has left.
“We have specified separate treatment arrangements for inpatient and outpatients,” notes DIR co-contributor Professor Zhang Li, MD, PhD. “And, to address the high patient volumes in Chinese hospitals, the guidelines recommend scheduling patient treatments on the same linac at different time slots to improve efficiency.”
Segmenting risk areas
Most RT centers are partitioned into several different areas (e.g., office area, diagnosis room, body immobilization room, treatment room, plan room, etc.). The DIR designates each area as “Clear Band,” “Semi-clean Area,” or “Contaminated Area” based on whether there is patient entry/contact. The personal protective equipment (PPE) varies in each area, with PPE in Contaminated Areas the most comprehensive, i.e., working cap, safety glasses, medical-use mask, protection suit, shoe covers, etc. All areas are subject to frequent disinfection and ventilation procedures, and a strict hand-washing protocol is mandated.
Staff education is key
“Because of the time RT staff spend in the center, it is their responsibility to carry out these guidelines diligently to safeguard not only patients, but themselves,” Professor Guangyuan says. “This is why the most important aspect is the DIR’s protection knowledge training, which includes self-learning, multimedia platforms, Covid-19 diagnosis and treatment guidelines, the ‘Seven-step hand-washing method’ and how to correctly wear and use PPE. All of this training is done via small-group teleconferences.”
Contingency plan for an RT patient with Covid-19
Despite maximum precautions to prevent coronavirus spread, there is still a risk that a radiotherapy patient has a suspected or confirmed case. Accordingly, the DIR developed a contingency plan to address this situation.
“If a Covid-19 case is found, all treatments need to stop, and the patient’s close contacts need to be determined, such as patients who were treated at the same or adjacent time slot and also the technicians,” he says. “These contacts need to be examined and isolated as required, and the treatment room needs to be disinfected and sterilized using ultraviolet radiation and other disinfectants, after which the RT shelter can re-open.
“All hospital patients – cancer patients in particular – and the medical staff that care for them need to be vigilant about how transmissible Covid-19 is,” Professor Li observes. “However, with the practices we’ve outlined in the DIR, that risk can be greatly minimized. The goal is near-zero risk.”
NOTE: Please ensure you are informed of and are following all the applicable guidelines and regulations at your location. This document contains information provided by third party sources to Elekta that does not necessarily represent the views of Elekta. Accordingly, third party information contained herein is provided “as is” with no guarantees of completeness, accuracy, usefulness, or timeliness.