Symmetry 4D image guidance enhances single isocenter SBRT for three lung metastases
Overview
This 68-year-old male patient underwent radical surgery for esophageal carcinoma in December 2016. In June 2017, he received intensity modulated radiation therapy (IMRT) to a supraclavicular lymph node metastasis, followed by chemotherapy (Xeloda and Nedaplatin) from August to October 2017. In June, 2018, a lung metastasis was successfully treated with Apatinib and S-1 chemotherapy.
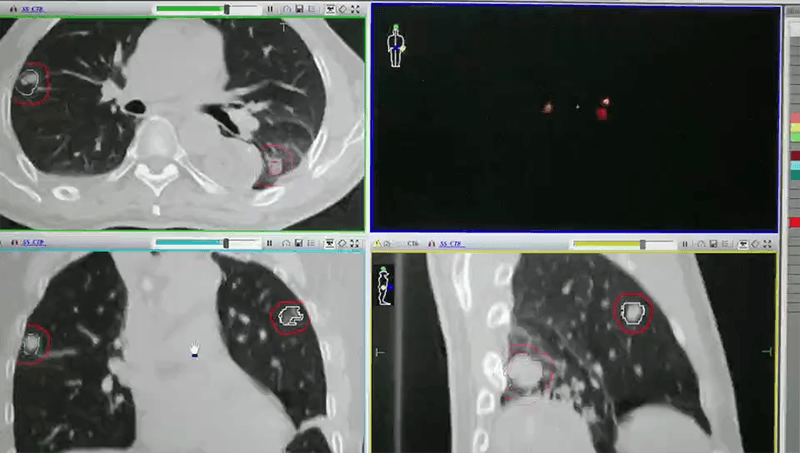
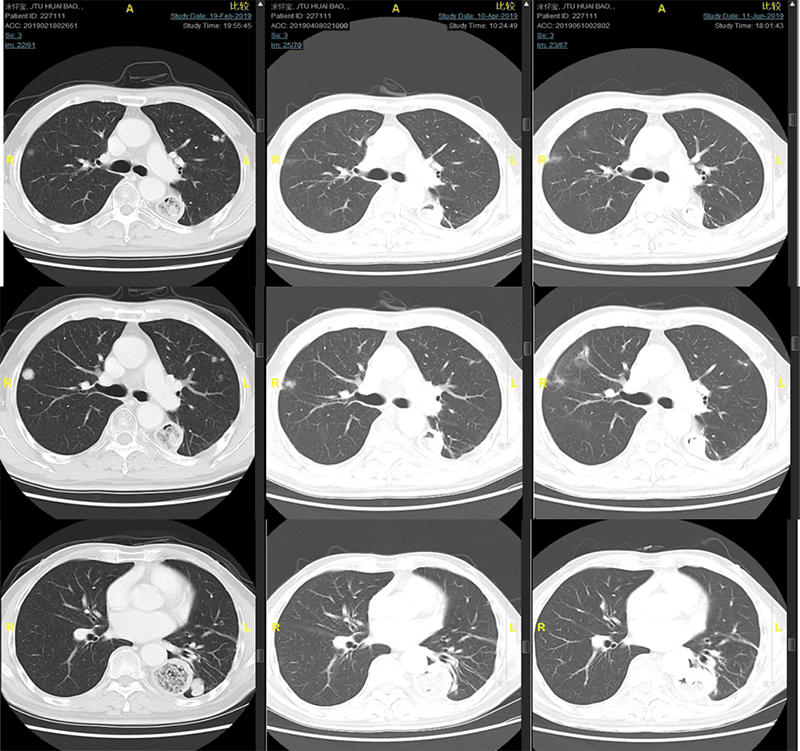
In February 2019, three new lung metastases were identified: one in the upper right lobe; one in the upper left lobe; and one in the lower left lobe (figure 1).
Prescription
This case presented challenges because of the distance between the three targets and the large, varying range of respiratory motion for each target. In addition, the three targets were in close proximity to different surrounding healthy tissues/OARs, such as the chest wall and intrathoracic stomach.
Considering this patient had received previous radiotherapy and chemotherapy, and the target volumes in the lung were small, it was decided to treat all three targets using one single-isocenter SBRT plan. Not only are the clinical outcomes for lung SBRT favorable, but the cost effectiveness of lung SBRT treatment, delivered over a shorter fractionation schedule, allows a reduction in treatment expenses by 66%.
Technique
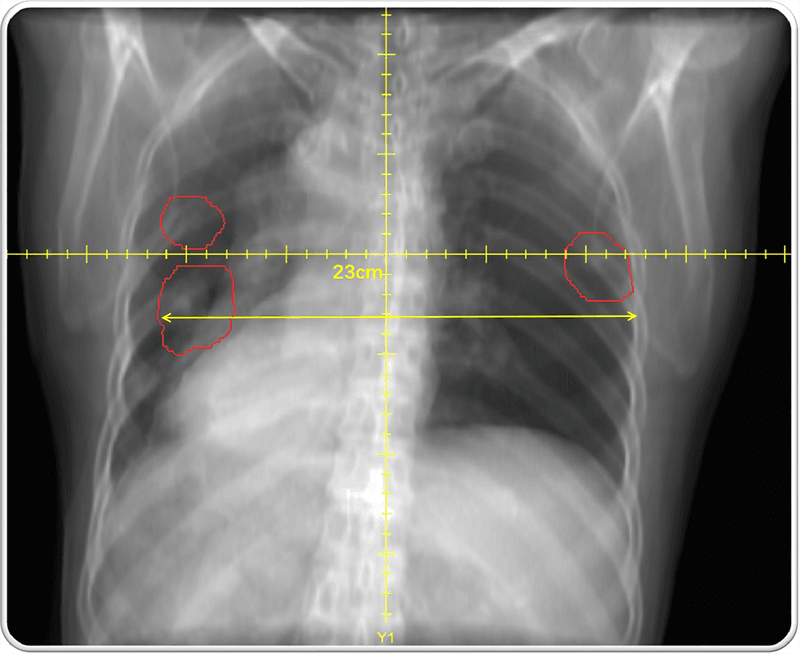
As the distance between the targets was 23 cm (figure 2), Versa HD (with the Agility MLC) was the only option to treat all three targets using one SBRT plan. This is due to Agility’s large treatment field with full-field 5 mm MLC leaf width resolution, its large MLC leaf interdigitation capability and its dynamic jaw tracking. In addition, Agility’s low leaf and jaw transmission protects healthy tissue by reducing inter-target dose.
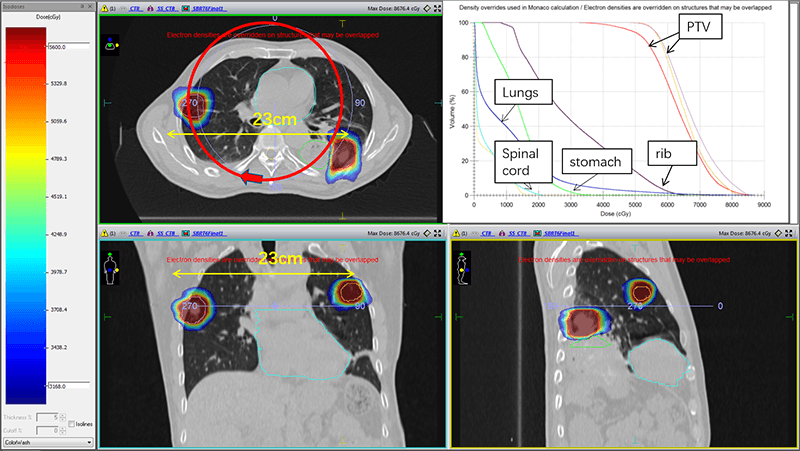
In the treatment of lung tumors, depending on tumor position, the PTV typically comprises a margin of 10-20 mm to account for respiratory motion. By expanding the volume irradiated, this increases dose to healthy lung tissue and, in this case, dose to the ribs also becomes a factor due to the close proximity of the tumors to the chest wall. However, with Symmetry, PTV margins can be reduced safely and effectively with confidence.
Symmetry provides better visualization of the tumor position throughout the entire breathing cycle. A time-weighted average position of the target is determined via 4D CBCT. This allows margin reduction by providing visualization of the entire tumor trajectory throughout the patient’s respiratory phases, thus sparing healthy tissue and OARs. Furthermore, intra-fraction 4D CBCT (Symmetry) allows real-time monitoring of tumor motion at the time of treatment, making sure that every target remains inside the ITV and PTV throughout treatment.
In this case, we compared a planning 4D CT image set (10 phases) and 4D CBCT (Symmetry) images to contour each ITV. Based on these 4D images, we were able to define a PTV margin of just 3-5 mm. A smaller PTV made treatment planning easier, allowing improved sparing of OARs, and Monaco’s Monte Carlo dose calculation accuracy ensured that dose to the chest wall was sharply improved.
A single isocenter, dual arc VMAT plan was generated using Monaco (figure 3) to deliver a total of 56 Gy to each of the three metastases over seven fractions, according to AAPM-RSS medical physics practice guideline 9a for SRS-SBRT.
The patient was immobilized supine with both arms raised, using BodyFIX® to reduce the range of patient movement dramatically.
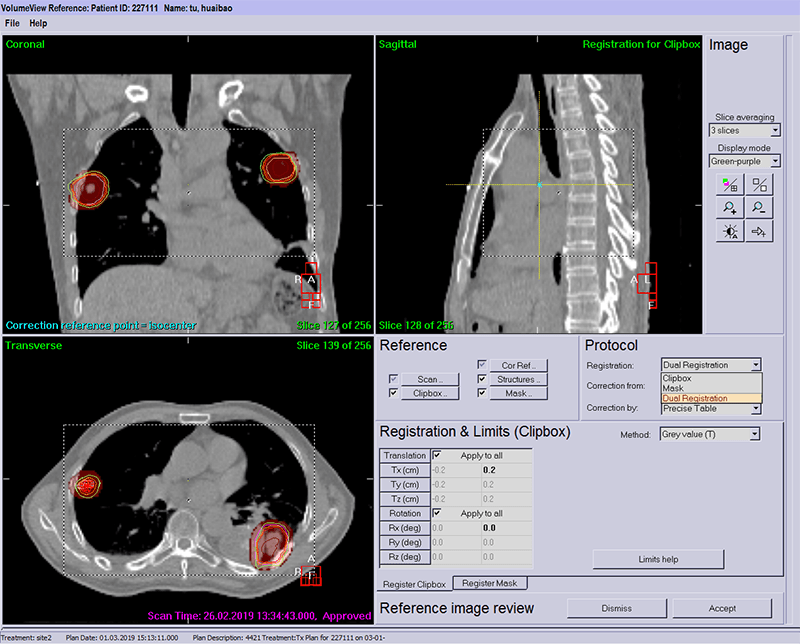
Before treatment, 4D CBCT (Symmetry) images were captured and, using Critical Structure Avoidance (CSA), all three targets were registered at the same time. Dual registration allows the protection of critical structures by allowing the simultaneous registration of both a designated OAR and the target. This allows for isocenter corrections based on either the OAR registration, target registration or a combination of the two, as well as providing an analysis of the relationship between them both. In this case, one of the targets is situated close to the stomach wall, which requires special protection (see figure 4).
Metrics: The distance between the target PTV and the 95% isodose line was measured on the treatment plan. This distance was used as the tolerance for position verification. Not only does Symmetry allow targets to be located accurately before treatment, but it also allows us to be sure that targets influenced by respiratory motion are within the ITV during treatment. Target movement data analysis for this patient is shown in table 1.
Table 1. Patient body movement data analysis
| Interfraction deviation | Intrafraction deviation | |||||
| Fraction | Tx | Ty | Tz | Tx | Ty | Tz |
| 1 | 0.11 | -0.99 | -0.30 | 0.10 | -0.11 | 0.00 |
| 2 | 0.09 | -1.16 | -0.47 | 0.13 | -0.02 | 0.05 |
| 3 | 0.08 | -1.13 | -0.29 | 0.14 | 0.22 | -0.16 |
| 4 | 0.30 | -1.24 | -0.03 | 0.10 | -0.04 | -0.07 |
| 5 | -0.25 | -1.22 | -0.27 | 0.31 | -0.40 | -0.01 |
| 6 | 0.70 | -1.33 | -0.21 | 0.15 | -0.32 | -0.08 |
| 7 | 0.34 | -0.80 | 0.05 | 0.16 | -0.07 | -0.04 |
| Mean ± SD | 0.27±0.22 | 1.15±0.19 | -0.23±0.15 | 0.15±0.07 | 0.16±0.15 | 0.05±0.05 |
The rapid delivery that could be achieved using Symmetry image guidance, VMAT and single isocenter, multi-target SBRT ensured a shorter treatment time, which reduced the risk of positioning errors.
Technical Planning Comments
The Jiangsu Cancer Hospital Department of Radiation Oncology began using Symmetry 4D image guidance for lung cancer in 2018. The department has adopted several motion management techniques, including respiratory gating, breath-hold techniques and optical surface management system (OSMS). Symmetry 4D image guidance technology is most often adopted for lung SBRT of pulmonary nodules or oligometastatic lesions that require real-time monitoring of tumor movement during treatment. CSA is used for critical structure protection and position verification, while intra-fraction Symmetry 4D image guidance is used for real-time tracking of respiratory motion during treatment delivery. This is particularly important with multiple targets, ensuring that each individual target is treated effectively.
In this case, Symmetry 4D CBCT provided high quality image guidance, allowing tumor position to be tracked during respiratory motion. This gave us the confidence to reduce PTV margins and allowed us to implement one SBRT plan for three lung metastases. This technique allowed us to improve departmental efficiency by shortening treatment delivery times, reducing the treatment course, and allowing multiple targets to be treated simultaneously and effectively. Symmetry scanning time was short and the workflow was easy.
CSA (which allowed us to register targets and critical structures) ensured that critical structures were well protected, effectively maximizing dose to the targets while minimizing dose to the surrounding critical tissues.
Report
Versa HD with Agility, Monaco treatment planning system, Symmetry 4D image guidance and CSA allowed us to treat this patient with three lung metastases successfully and efficiently, using single isocenter, multi-target lung SBRT. The patient tolerated the treatment well, with no toxicity or side effects reported at the time of treatment or at three month follow up. Follow up imaging at one and three months after treatment demonstrate significant treatment effect and the patient’s condition is greatly improved (figure 5). Follow up with the patient continues.
References
- Wolthaus, JWH et al (2008) Comparison of different strategies to use four-dimensional computed tomography in treatment planning for lung cancer patients. Int. J. Radiation Oncology Biol. Phys. 70(4):1229–1238.
- Halvorsen, PH et al (2017) AAPM-RSS Medical Physics Practice Guideline 9.a. for SRS-SBRT. J Appl Clin Med Phys 18(5):10-21.
- Videtic, GMM et al. (2017) Stereotactic body radiation therapy for early-stage non-small cell lung cancer: Executive Summary of an ASTRO Evidence-Based Guideline. Pract Radiat Oncol 7(5):295-301.
- Guckenberger, M et al (2017) ESTRO ACROP consensus guideline on implementation and practice of stereotactic body radiotherapy for peripherally located early stage non-small cell lung cancer. Radiother Oncol 124(1):11-17.
- Nyman, J et al (2016) SPACE - A randomized study of SBRT vs conventional fractionated radiotherapy in medically inoperable stage I NSCLC. Radiother Oncol 121(1):1-8.
- Swaminath, A et al (2017) Canadian Phase III Randomized Trial of Stereotactic Body Radiotherapy Versus Conventionally Hypofractionated Radiotherapy for Stage I, Medically Inoperable Non-Small-Cell Lung Cancer - Rationale and Protocol Design for the Ontario Clinical Oncology Group (OCOG)-LUSTRE Trial. Clin Lung Cancer 18(2):250-254.
Jiangsu Cancer Hospital
Institution: Jiangsu Cancer Hospital
Nanjing, Jiangsu Province, China
Contributors: Qian Pudong, Director, Radiation Oncologist
Zhang Siyu, Medical Physicist
Ming Xuezhong, Radiation Therapist
Jiangsu Cancer Hospital is the center for cancer prevention, treatment, research and education in Jiangsu Province. It has been on the list of “National Best Oncology Reputation Ranking” published by the Medical Management Research Center of Fudan University for seven years and, in 2015, it became one of the top 100 “Best Hospitals in China”.
The Jiangsu Cancer Hospital Radiation Oncology department was established in 1961 and currently employs 77 physicians, 16 medical physicists, 47 radiation therapists and 140 specialist nursing staff. With an average patient throughput of around 5,000 per year, the department has six inpatient areas, including head and neck, abdomen, thorax and gynecological oncology. The department is equipped with two Elekta Versa HD linacs, in addition to Varian UNIQUE, 600CD, VitalBeam and TrueBeam linacs.
