Single isocenter high definition dynamic radiosurgery (HDRS) for multiple brain metastases
Case: Stage 4 hard palate osteosarcoma with multiple brain metastases.
Overview
This 49-year old male patient was previously diagnosed with hard palate osteosarcoma with lung metastasis in December 2013. At that time, the patient was treated with multiple lines of chemotherapy, including cisplatin/doxorubicin/avastin and high dose methotrexate, with a resection and radiotherapy to the primary site.
In April 2017, PET-CT demonstrated fluorodeoxyglucose (FDG) avid soft tissue thickening in the right cheek, inferior temporal fossa, along the anterior maxilla margin and zygoma. This appeared generally stable in extent, but with mixed metabolic response. PET-CT also revealed progressive lung metastases with increase in size and metabolic activity. A left lower lobe lesion measured 2.3 x 3.5 cm and a right upper lobe lesion measured 4.7 x 3.8 cm.
Additional suspected metastases were observed, as follows: interval new FDG avid lesions were present in the left gluteal muscle; interval new FDG avid calcific foci were seen in the right pectoralis major muscle and right soleus muscle; there was an interval new FDG avid calcified lesion in the right occipital lobe, with associated adjacent vasogenic edema; and there was an interval new FDG avid lesion in the right proximal femur.
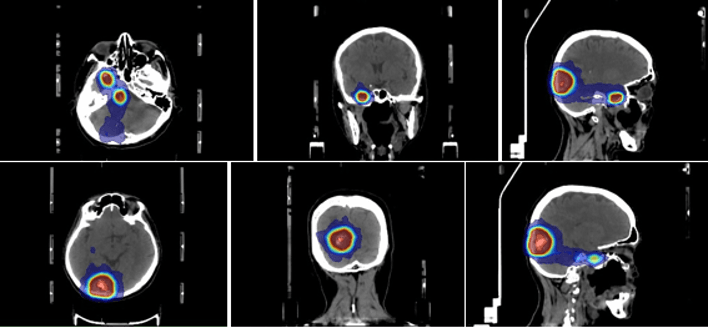
The lung metastases were treated using stereotactic body radiotherapy (SBRT) in May 2017. The patient received 45 Gy over five fractions to each lesion in the left and right lungs independently, delivered on alternate days. PET-CT assessment in October 2017 revealed that the lung metastases were larger in size (left lung: 2.6 x 3.4 cm; right lung: 5.5 x 4.3 cm) but showed decreased metabolic activity. The patient also received immunotherapy with palbociclib and pembrolizumab. An MRI scan of the brain (multiplanar sequences, including post-gadolinium sequences), performed in October 2017, revealed an ovoid extra-axial, dural-based mass in the right occipital lobe, measuring 3.3 x 2.7 cm, associated with areas of internal susceptibility and surrounding oedema (figure 1a). The MRI also revealed a smaller enhancing dural nodule (0.7 x 0.6 cm) in the temporal lobe located in the floor of the right middle cranial fossa, with surrounding oedema, and an intra-axial node (0.6 x 0.6 cm) in the right hemi-pons, with surrounding oedema (figure 1b). Given the submitted diagnosis of osteosarcoma, these lesions were suspected brain metastases.
MRI scan of brain metastases
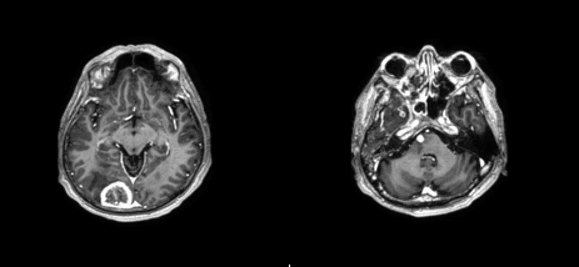
a) (left) Lesion in the right occipital lobe
b) (right) Lesions in the right hemi-pons and right
temporal lobe
Clinically, the patient was experiencing occipital right sided headache and subjective diplopia. Following discussion about potential side effects, the patient was agreeable to stereotactic radiosurgery (SRS), to be delivered to the three targets in the brain in three fractions.
Device: Versa HD, HexaPOD evo RT
Beams
Prior to the first treatment, the brain SRS plan check and QA check was performed using Mobius3DFX QA software and a ‘20 cm slabs’ phantom with Gafchromic EBT3 film concurrently. Mobius3DFX has an independent beam model based on collapse cone dose calculation algorithm, to check target coverage and OAR DVH limits. A dose grid of 2 mm and 3D gamma criteria of 3%/2mm ≥ 95% were used.
Following this, triple channel film dosimetry analysis was performed with lateral response artifact correction. At this center, a pass rate of >95% has been achieved with 2D gamma criteria of 2%/2 mm using FilmQAPro software and with 3D gamma criteria of 3%/2 mm using the Mobius3DFX software. Quality assurance using the Mobius3DFX software was also performed for the remaining fractions using log files.
Treatment commenced on the 30th October 2017, with the subsequent fractions delivered on the 1st and 3rd November 2017. Prior to each fraction, an XVI VolumeView™ image was performed for isocentric and anatomical verification; with automatic bone registration completed, translation and rotational errors calculated, and manual adjustments made as required. HexaPOD™ table shifts for each day are shown in the table below.
HexaPOD table shifts prior to treatment delivery
| Translation (cm) | Rotation (°) | |||||
| Date | X | Y | Z | X | Y | Z |
| 30.10.2017 | -0.07 | 0.17 | 0.18 | 0.7 | 0.01 | 0 |
| 01.11.2017 | -0.22 | 0.09 | 0.11 | 0.1 | 1.4 | 1.3 |
| 03.11.2017 | -0.02 | -0.02 | 0.14 | 0.7 | 0.2 | 0.2 |
Each fraction was delivered within a 15-minute timeslot. Total treatment time for each consecutive fraction was 12 minutes, 12 minutes and 14 minutes.
DVH
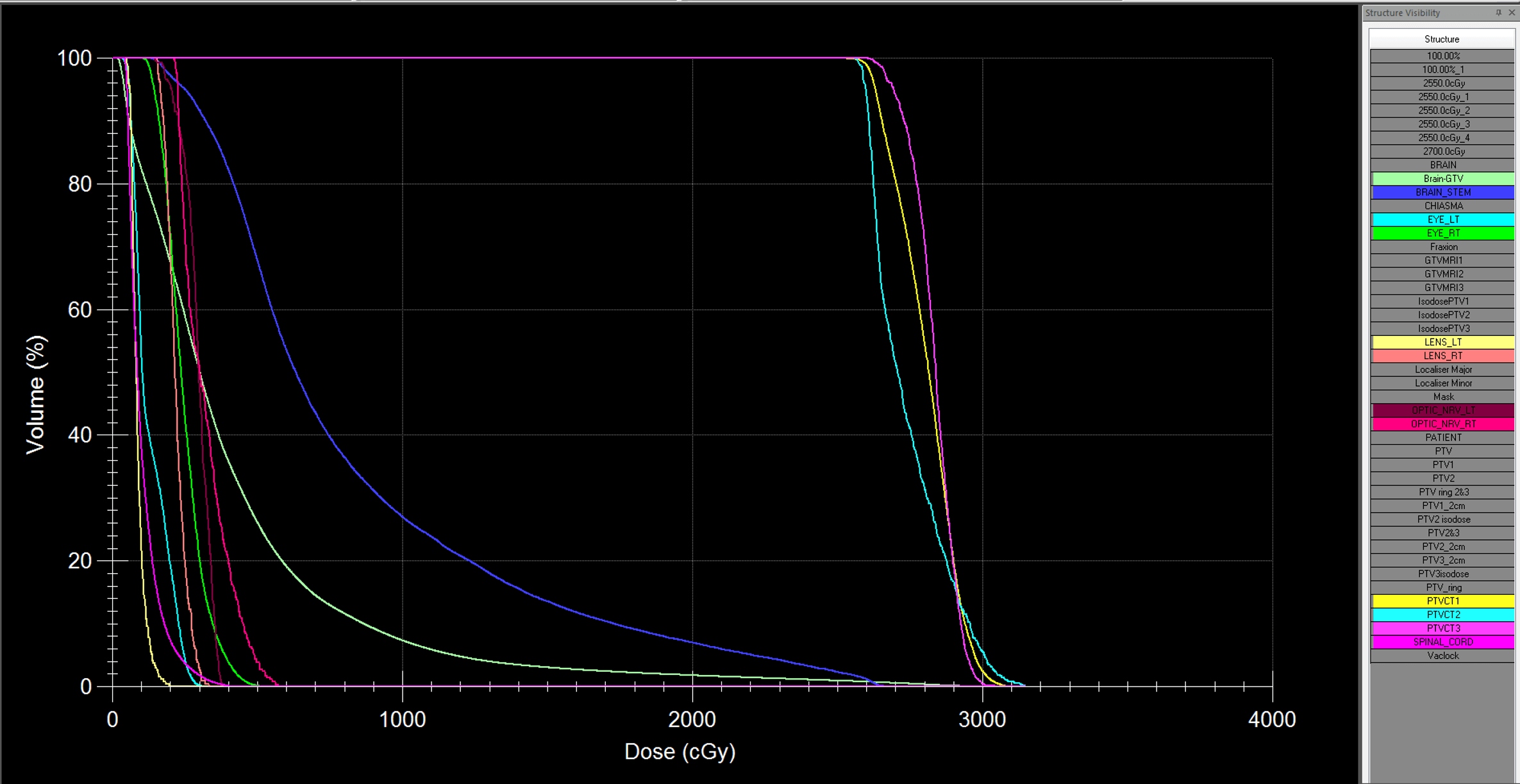
Metrics
Report
A post-treatment brain MRI scan was performed on 25th January 2018, three months following the previous scan. The ovoid extra-axial, dural-based mass in the right occipital lobe could be seen, associated with areas of internal susceptibility and surrounding oedema. Measuring 3.4 x 2.6 cm, this lesion appeared stable in size, compared to the previous scan, with continued surrounding oedema. However, there appeared to be decreased peripheral vascularity around this lesion. The smaller enhancing dural node in the right temporal lobe also appeared stable in size, measuring 0.7 x 0.6 cm, with decreased peripheral enhancement compared to the prior study. Similarly, the intra-axial node in the right hemi-pons, measuring 0.6 x 0.6 cm, appeared stable in size with decreased internal enhancement.
Although there is little change in size of these three brain metastases, the interval decease in enhancement compared to the previous pre-treatment MRI scan is suggestive of disease response. For frameless brain SRS/SRT, immobilization of the head with a stereotactic grade mask, such as Fraxion, is critical and enabled us to position the isocenter with minimal error. In our experience, the shifts required for longitudinal and pitch errors are the largest. This is likely due to sag on the treatment table and/or possible head tilt/motion. The use of a good IGRT workflow and the HexaPOD evo RT patient positioning system, with sub-millimeter patient positioning accuracy, enabled corrections to be made in six degrees of freedom, which was of particular value for the pitch error. The use of Monaco, with the rapid and accurate Monte Carlo dose calculation algorithm, together with the high available modulation that can be achieved using Monaco and Agility (where the mechanism of the MLC leaves and the dynamic jaws produce a ‘virtual leaf width’ of as little as 1 mm) allows highly accurate dose calculation, even for very small targets (~1.0 cc). These features eliminate the need for stereotactic cones or add-ons for treating single small targets.
A two-millimeter margin was used to account for factors, such as potential patient movement in the mask, small targets, or targets distant (> 4cm) from the isocenter. Furthermore, in a retrospective study, Choi et al found that local control improved with a two-millimeter margin compared to no margin1.
1. Choi, C.Y.H et al (2012) Stereotactic Radiosurgery of the Postoperative Resection Cavity for Brain Metastases: Prospective Evaluation of Target Margin on Tumor Control. Int J Radiation Oncol Biol Phys 84(2): 336-342.
For small field treatments delivering high doses per fraction, it is advantageous to use high dose rate delivery at some segments. Versa HD high dose rate (6 MV FFF) is able to deliver 1400 MU/min, which enables faster treatments and, thus, reduces the risk of intrafractional motion. The combined accuracy of Monaco, Versa HD (with FFF) and HexaPOD, along with the use of a 2 mm GTV margin, enabled us to use a single isocenter, multi-focal SRS technique to treat multiple brain metastases as the primary option for this patient, instead of whole brain radiotherapy. This combination offers a much more versatile and efficient treatment compared to other brain SRS techniques, which are mainly designed for single or few targets, allowing all three targets to be treated within three standard 15-minute timeslots, with improved patient comfort and reduced risk of intra-fraction patient movement.