Active Breathing Coordinator™ and MotionView™ help to spare the heart and left lung in left breast cancer radiotherapy
Institution: The First Affiliated Hospital of Xi’an Jiaotong University (XJTU)
Location: Xi’an, Shaanxi, China
Overview
Clinical application of moderate deep inspiration breath-hold (mDIBH) in left breast radiotherapy Active Breathing Coordinator™ and MotionView™ help to spare the heart and left lung in left breast cancer radiotherapy.
Prescription
In October 2019, a 48-year-old female patient presented with a chestnut-sized mass in the lower-inner quadrant of the left breast. The mass was firm with no swelling or nipple discharge, and there was no headache or other obvious signs of discomfort. A fibroadenoma was suspected following breast ultrasound. Biopsy later revealed that the mass was a mucinous carcinoma.
The patient elected to have breast-conserving surgery in December 2019. Pathology of the mass confirmed breast mucinous adenocarcinoma (Grade I). Following breast-conserving surgery, there was a reactive hyperplasia in the left front lymph node.
Technique
After discussion between experts in the radiotherapy department, and considering the patient’s treatment history and current situation (such as her normal lung function), it was decided to treat the patient using a moderate DIBH (mDIBH) technique.
Left-sided breast radiotherapy is associated with certain challenges. Firstly, respiratory motion is a challenge to the accurate delivery of dose to the target and, secondly, it is important to minimize dose to nearby critical structures, such as the heart and left lung. All things considered, the clinicians decided to adopt a moderate deep inspiration breath-hold (mDIBH) technique to maximize dose and accuracy to the target, while minimizing dose to the heart and left lung.
For simulation and treatment, the patient was positioned supine with arms raised in the BreastSTEP™ patient positioning device. Prior to simulation, the patient received some training on how to hold her breath for mDIBH using the Elekta Active Breathing Coordinator™ (ABC) version 3.0. After monitoring her normal breathing pattern, the inhalation threshold was set to 1.2 liters and the breath-hold time was set to 28 seconds. The patient was able to observe her real-time respiratory amplitude and threshold level through a speculum, and so could control the deep inspiration to the threshold level on her own.
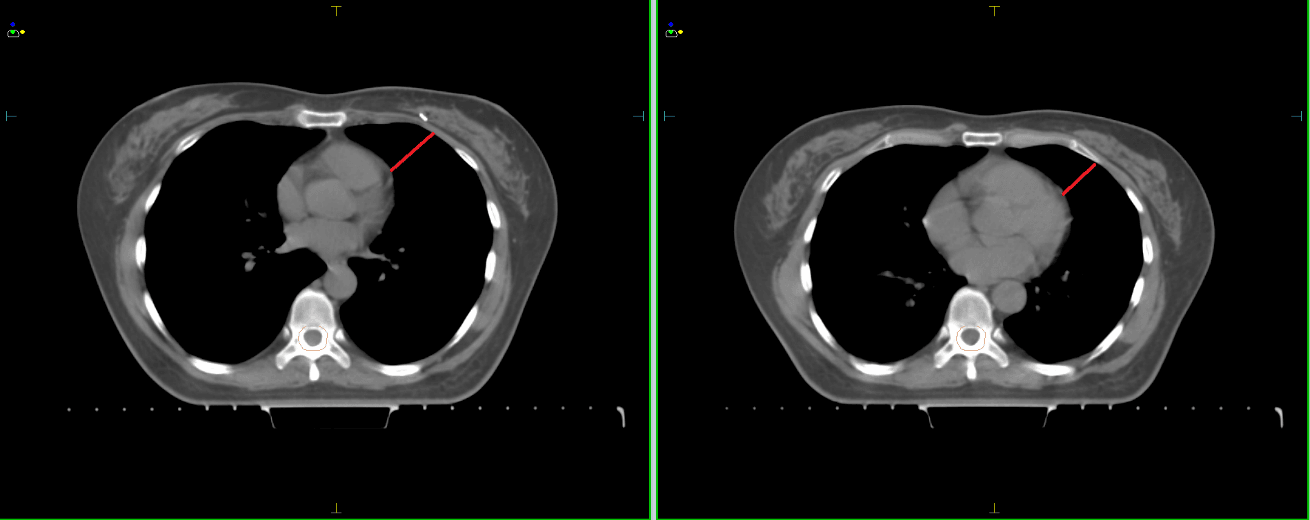
CT images were captured during mDIBH. Since the scan time was around 15 seconds, only one breath-hold was required for simulation. In order to clearly see the benefits of mDIBH for this patient, CT images were also captured while the patient was breathing freely (figure 1). The mDIBH CT image shows a distance between the heart and the chest wall of 4.02 cm. With the patient in free breathing, this distance is 2.82 cm and so mDIBH technology expanded the distance by 1.2 cm.
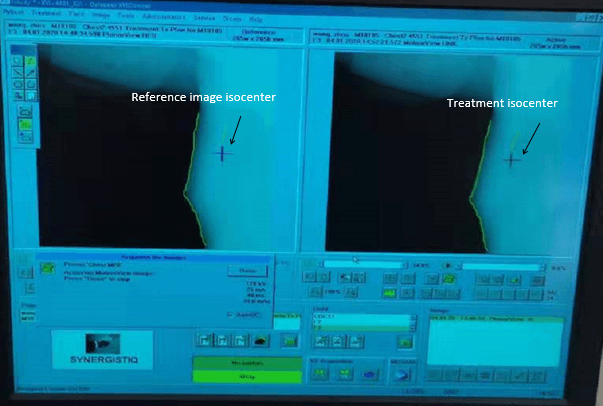
CBCT imaging of the patient was used to improve the accuracy of patient positioning. Before treatment, a quick XVI scan (< 40 seconds) was performed during mDIBH to make sure the treatment isocenter and the planned target isocenter were highly aligned. Following the necessary corrections, the patient was ready to receive the treatment. The treatment was delivered using Elekta Versa HD.
During treatment, the combination of ABC and the Response gating interface ensured that beam-on only occurred during the breath-hold and that the beam was off while the patient was breathing freely. In this way, the patient did not receive any unexpected dose. The mDIBH process was repeated for each fraction until the required dose was delivered.
In addition, XVI MotionView™ intra-fraction image guidance was also adopted during treatment to monitor patient respiratory movement in real time (figure 2).
Metrics
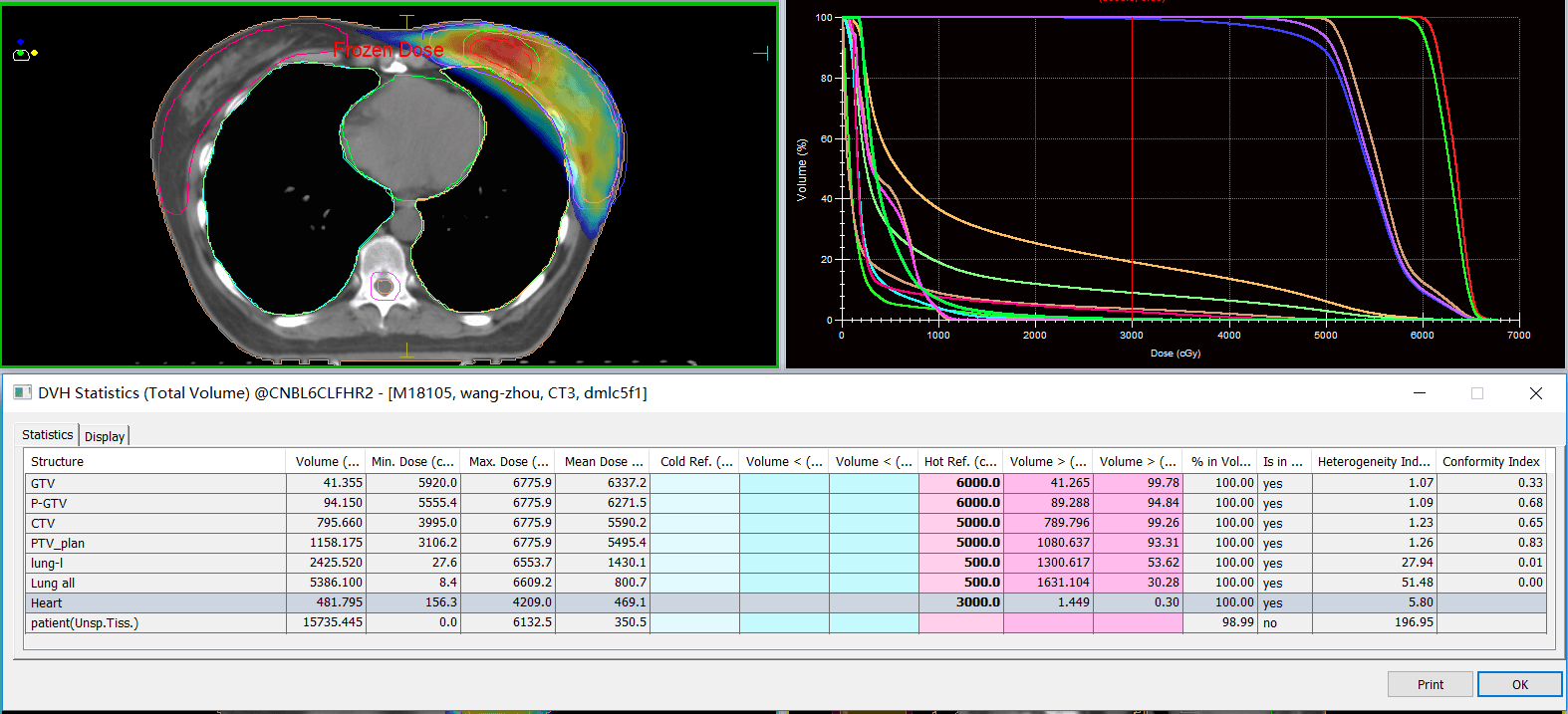
The prescribed dose was 50 Gy to the PTV and 60 Gy to the P-GTV, delivered over 25 fractions. Prescribed and actual doses and constraints are shown in table 1.
| Prescription/constraints | Actual plan | ||
| Target | PTV | 5000 cGy/25# Cover 95% volume | 5000 cGy Cover 94.84% volume |
| PGTV | 6000 cGy/25# Cover 95% volume | 6000 cGy Cover 99.78% volume | |
| Critical structures | Heart | Dmean <500 cGy | Dmean = 469.1 cGy |
| Lung | V5 <55%, V20 <25%, V30 <20% | V5 = 53.62%, V20 <24.94%, V30 <18.58% | |
| Spinal cord | Dmax <2000 cGy | Dmax = 1115.6 cGy | |
Table 1. Prescribed (left) and actual (right) dose and constraints
| Free-breathing | ABC mDIBH | |
| Patient lung volume | 1232.470 cc | 2425.520 cc |
| Average doses to heart | 868.5 cGy | 469.1 cGy |
| Heart V30 | 7.64% | 0.3% |
| Heart max doses | 5479 cGy | 4209 cGy |
| Average doses to lung | 1785.8 cGy | 1430 cGy |
| Left Lung V20 | 31% | 25% |
| Left Lung V30 | 26% | 19% |
Table 2. Comparison of lung volume and dose to healthy anatomy between mDIBH and free-breathing plans
To further improve plan quality and treatment efficiency, a high dose rate beam (6 MV FFF) and Monaco DMLC fixed field dynamic IMRT were used. The plan included a total of five fields at gantry angles of 290°, 340°, 20°, 100° and 132°. Planned dose distributions and DVH statistics are shown in figure 3.
The mDIBH plan was compared to a free-breathing plan to assess the level of critical structure sparing (figures 4 and 5). It was shown that mDIBH using ABC was able to increase the distance between the heart and the radiation field (figure 4) and to reduce dose to the heart and the left lung (figure 5).
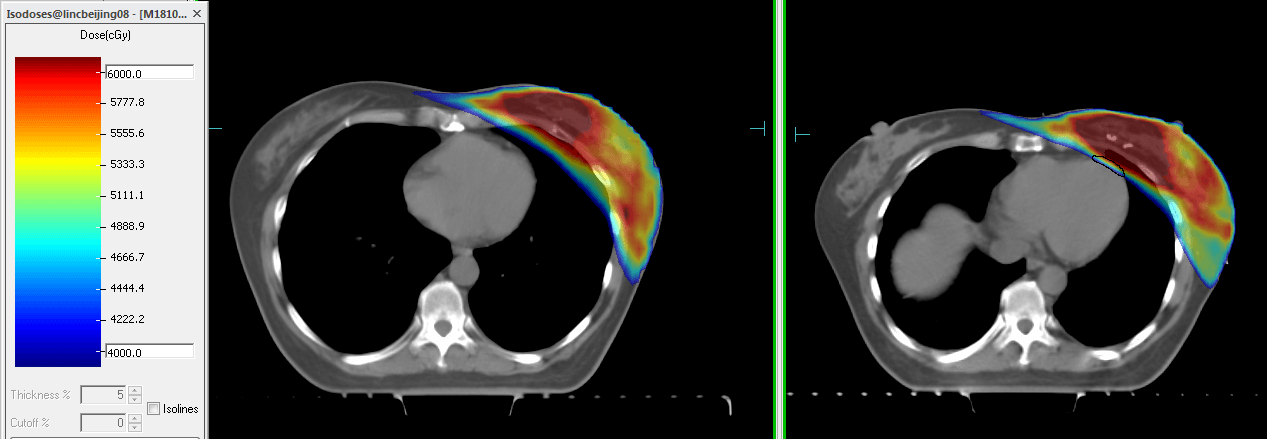
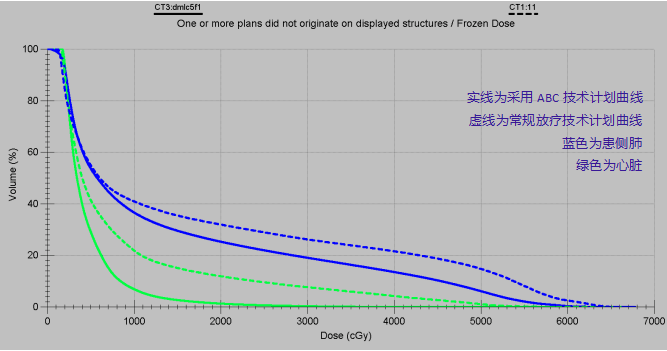
Adopting the mDIBH technique with ABC almost doubled the volume of the left lung, pushing the heart away from the radiation field. This effectively decreased the dose delivered to the heart, thus reducing radiation-related toxic side effects.
Pre-treatment plan quality assurance was performed using Delta4 3D verification. The results met all clinical requirements and the plan was approved.
Technical planning comments
This case demonstrates that the clinical application of a moderate deep inspiration breath-hold (mDIBH) technique offers benefits to the treatment of left-sided breast cancer patients. The deep inspiration expands the thorax, increasing the distance between the breast and the heart, while effectively reducing dose to both the heart and left lung.
Our radiation department is equipped with the Elekta Active Breathing Coordinator™ (ABC), which assists the patient in a comfortable, consistent DIBH. The breath-hold remains in the patient’s control and beam gating is achieved using the Response gating interface.
This case also benefited from the accuracy of Monaco’s gold-standard Monte-Carlo dose calculation algorithm and the advanced Versa HD linac, with its fully integrated, high-speed, highly accurate Agility MLC. Agility ensures efficient coverage of the targets, with its 160 interdigitating 5 mm leaves and rapid leaf speed (up to 6.5 cm/s). In addition, its extremely low leaf transmission (< 0.5%) better protects healthy tissue.
Report
The adoption of mDIBH for this left-sided breast cancer treatment decreased dose to the heart and left lung, thus lowering heart toxicity and reducing the risks of mid to long-term radiation-related complications.