GKRS for pediatric brain mets Cleveland Clinic
Case: Gamma Knife Radiosurgery (GKS) for pediatric brain metastases.
Contributor: James R. Broughman, MD; Erin S. Murphy, MD, Cleveland Clinic, Department of Radiation Oncology.
Overview
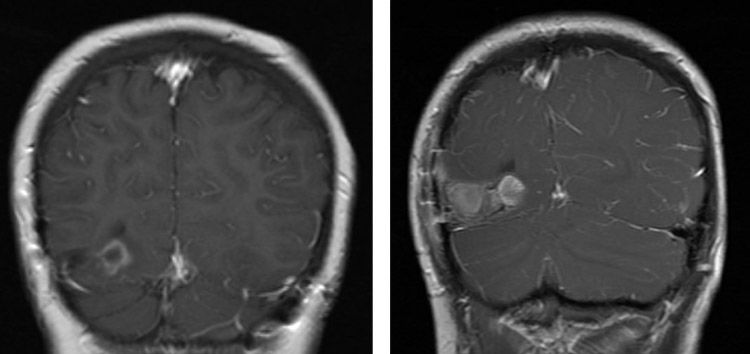
A 13-year-old male who initially received chemotherapy and surgery for Ewing sarcoma localized to left proximal humerus in 2017; developed metastatic disease in 2019. This included 2 calvarial and 2 brain metastases.
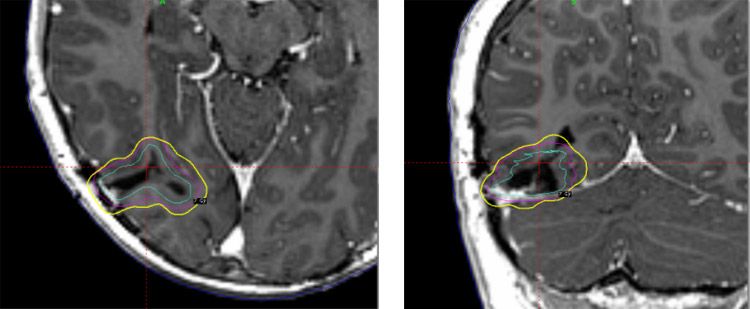
Metastasis 1: Right occipital: Volume 8.8 cm3
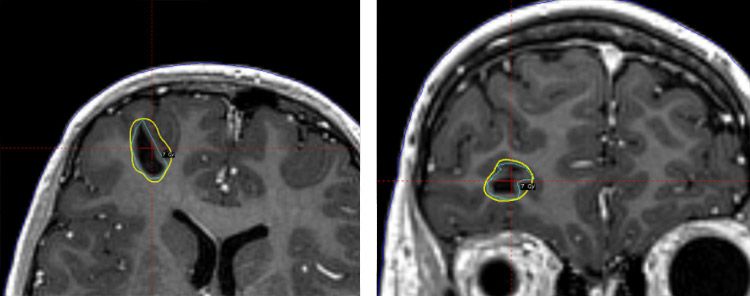
Metastasis 2: Right frontal: Volume 1.3 cm3
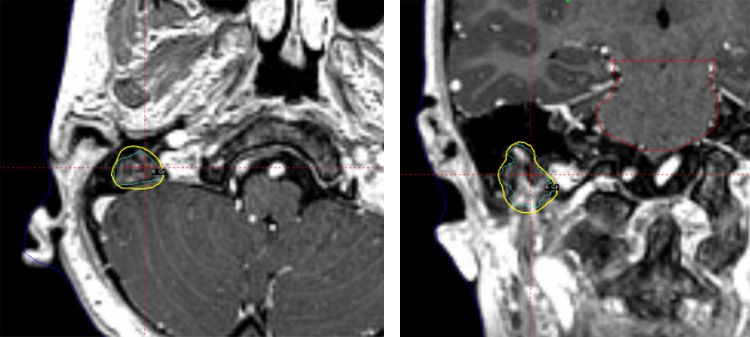
Metastasis 3: Right mastoid: Volume: 1.9 cm3
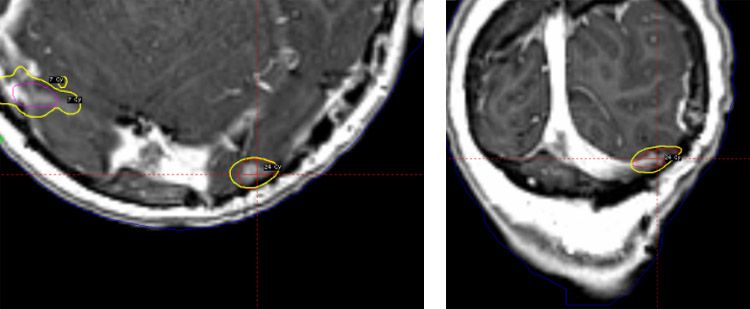
Metastasis 4: Left occipital: Volume: 0.3 cm3
- Median GTV Volume: 1.6 cm3 (range 0.3 -8.8 cm3)
- Total GTV volume: 12.2 cm3
Why Gamma Knife radiosurgery was chosen
In appropriately selected candidates, GKRS provides excellent local control while minimizing the neurocognitive toxicity associated with whole brain radiation therapy. The ability to deliver fractionated radiosurgery allows for effective tumor control while minimizing toxicity, particularly for large tumors or tumors abutting critical structures. Because less healthy tissue is affected, patients can have fewer side effects during and after treatment, such as headaches, fatigue, nausea, decreased appetite, hair loss and progressive neurological symptoms. There is also potential for reduced late effects, including neurocognitive impact, endocrine deficits, craniofacial growth changes, hearing loss and secondary malignancy.
Treatment protocol
The patient underwent salvage chemotherapy first and then this was followed by Gamma Knife radiosurgery.
Due to anxiety issues, the patient underwent mask-based Gamma Knife treatment under anesthesia. The thermoplastic mask was modified to allow passage of endotracheal tube. Three metastases were treated in five sessions over seven days while one small metastasis was treated in a single session. A total of 37 shots were utilized.
- Right occipital: 35 Gy/5x. 11 shots.
- Right frontal: 35 Gy/5fx. 10 shots.
- Right mastoid: 30 Gy/5fx. 13 shots.
- Left occipital: 24 Gy/1fx. 3 shots.
| Target Name | Target Location | Volume [cc] | Max. Dimension [cm] | PD [Gy] | IDL % | Coverage % | PIV/TV | # Shots | Plugs | Max. Dose | MD/PD | Complexity | Gradient Index |
| Right occ 2mm margin | Right occ 2mm margin | 8.782 | 3.29 | 35 | 53 | 100 | 1.439 | 11 | N | 13.2 | 0.377 | Simple | 2.8 |
| Right frontal | Right frontal | 1.297 | 2.2 | 35 | 51 | 100 | 1.534 | 10 | N | 14.1 | 0.403 | Simple | 2.7 |
| Right mastoid | Right mastoid | 1.938 | 2.31 | 30 | 62 | 100 | 1.707 | 13 | N | 9.7 | 0.323 | Simple | 2.4 |
| Left Occ | Left Occ | 0.337 | 1.63 | 24 | 51 | 100 | 2 | 3 | N | 47.1 | 1.963 | Simple | 3.33 |
Single fraction SRS is associated with worse local control for large lesions, so fractionated SRS is often utilized to improve local control while maintaining low rates of toxicity. Fractionated SRS was utilized for the right mastoid lesion to minimize toxicity to the adjacent facial nerve and the larger parenchymal metastases.
Results
- The Patient tolerated GKRS well.
- At 18 months follow-up, local control of treated lesions is 100%
- No symptomatic radiation necrosis or neurocognitive decline was noticed
- The patient subsequently developed 2 new brain metastases (0.5 cm3 in Right temporal lobe and 1.9 0.5 cm3 in Right parietal lobe). In October 2020, these new metastases were successfully treated using GKRS. There is currently no evidence of disease.
Concluding Remarks
“Gamma Knife radiosurgery is an underutilized tool for our younger patients. Gamma Knife Icon has
expanded the utility of GKRS in this population due to the ability to fractionate treatments which minimizes
toxicity while maintaining excellent local control.”
- Dr. Erin Murphy