A common cancer and a continuing challenge
Each year, millions of women are diagnosed with breast cancer, making it one of the most common cancers worldwide1. Although outcomes continue to improve, access remains uneven and many patients still face risks of long-term cardiac or lung effects. Radiotherapy, delivered through external beam or brachytherapy, plays a central role across early-stage, locally advanced, and recurrent disease, helping reduce local recurrence whilst preserving breast appearance, and quality of life.3
Radiotherapy plays a vital role in the overall management of early-stage, locally advanced, or metastatic breast cancer.2
of breast cancer patients
should receive radiotherapy2
Proven precision that protects the heart
Key clinical studies show that image-guided radiotherapy and brachytherapy improve accuracy, safety, and long-term outcomes for patients with breast cancer.
One-week treatment proven effective
The FAST-Forward trial confirmed that a five-fraction, one-week course of treatment is as safe and effective as the three-week standard. This increases the number of patients that can be treated, reduces patient travel and maintains tumor control.12, 13
Daily adaptation for consistent protection
Using daily imaging, motion management, and automation, adaptive workflows help you adjust for changes in breast contour, fluid-build up after surgery, and chest-wall position. This maintains coverage while reducing dose to the heart and lungs.8, 9, 11
Expanding non-surgical options
Stereotactic body radiotherapy (SBRT) is being explored as a preoperative option to reduce tumor size and as a curative option for patients unable to undergo surgery, particularly among certain elderly groups.4, 5, 8
Complementary precision with brachytherapy
Image-guided interstitial breast brachytherapy enables highly conformal dose delivery to the tumor bed for partial breast or boost treatment, while limiting dose to organs at risk, including the heart and lungs6. In selected patients, very accelerated partial breast irradiation can reduce treatment time without compromising outcomes.7
How adaptive radiotherapy helps you respond to clinical changes
| Your challenge | Adaptive helps you... |
| Daily changes in breast contour, fluid build-up, or swelling | Re-image and adapt plans to sustain target coverage and protect the heart and lungs.8, 9 |
| Cardiac and lung sparing in left-sided disease | Personalize setup and plan margins daily to minimise dose to organs at risk.8 |
| Respiratory motion and chest-wall movement | Combine gating and adaptive verification to ensure accuracy of every fraction.8, 9 |
| Treatment burden and capacity constraints | Deliver validated five-fraction hypofractionated regimens safely and efficiently.11, 12, 13 |
| Patients unsuitable for surgery | Use adaptive SBRT to achieve local control in curative or palliative settings.4, 5, 7 |
| Need for dose escalation or re-irradiation | Combine adaptive radiotherapy with image-guided brachytherapy for safe, conformal dose escalation.6, 7 |
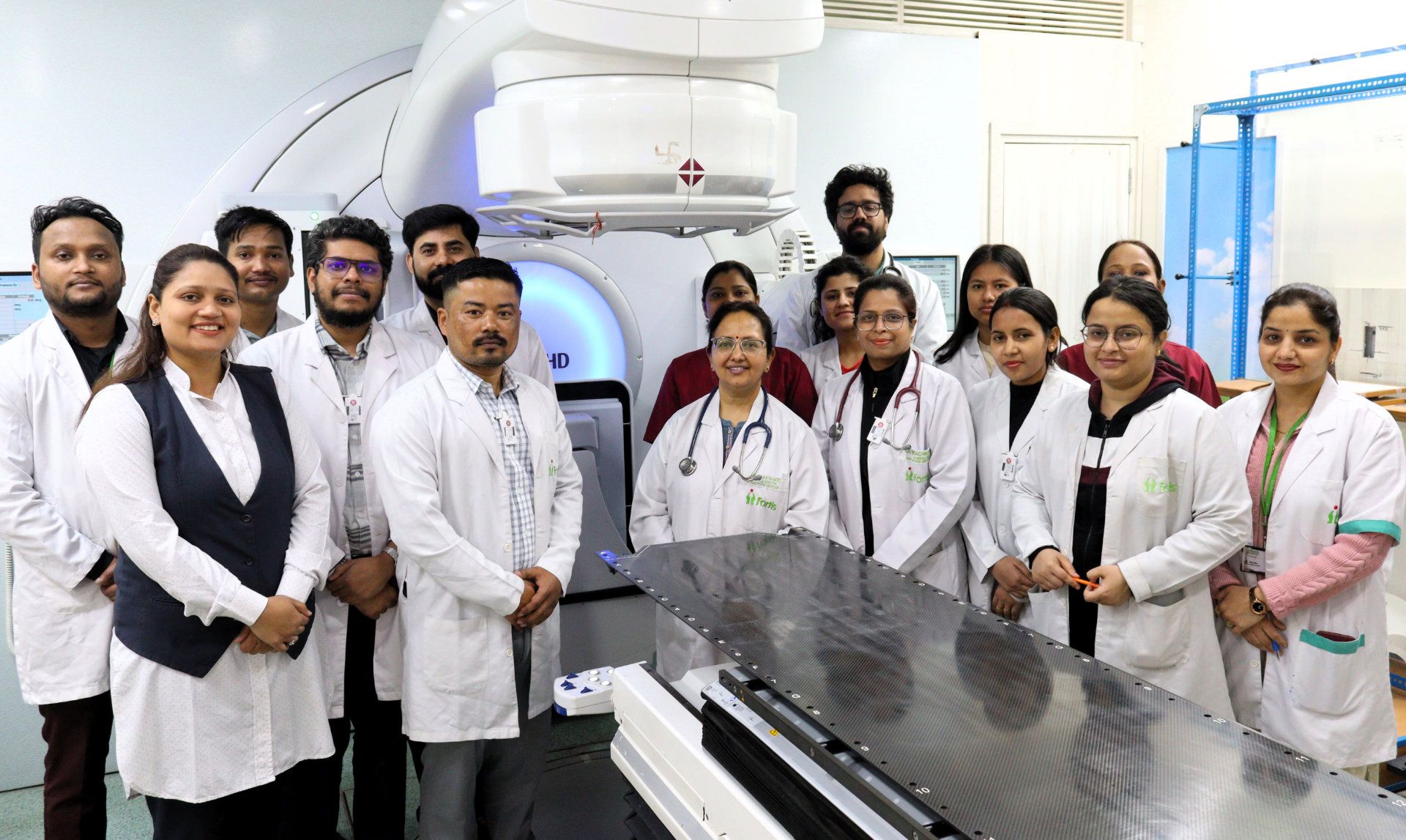
Clinics are already adapting and redefining what’s possible
Nobody does adaptive like Elekta
Every breast cancer case presents its own challenges, from daily anatomical changes to the need to protect the heart and lungs. Across MR- and CT-guided adaptive radiotherapy and image-guided brachytherapy, Elekta helps you adapt every fraction to the patient in front of you. We work closely with care teams globally to support treatments that help preserve breast appearance, minimize side effects, and ensure each patient receives precise and compassionate care.

Designed for precision that protects the heart
For many patients, left-sided disease brings the heart and lungs close to the treatment area. Adaptive planning lets you personalize treatment to the day’s anatomy, maintain coverage, and keep dose to critical organs as low as reasonably achievable. When dose escalation is needed, image-guided brachytherapy complements external beam radiotherapy to balance local control, breast appearance, and long-term protection.8, 9, 11
Adapting every fraction to protect the breast and vital organs
Breast anatomy can change significantly during treatment because of fluid build-up after surgery, swelling, or movement of the chest wall. Adaptive workflows let you visualize and adjust to these changes, maintaining accuracy and reducing dose to nearby organs. With adaptive you can:
Maintain accuracy throughout treatment
Re-optimize plans as anatomy evolves to sustain target coverage.
Protect the heart and lungs
Adapt to daily setup and motion variations to keep cardiac and lung doses as low as possible.
Deliver shorter, confident treatments
Deliver validated five-fraction regimens with confidence, supported by daily imaging and automation.
Combine modalities for optimal outcomes
Boost external beam radiotherapy with image-guided brachytherapy to achieve control with minimal toxicity.
Share your thoughts
We're asking how centers are approaching adaptive radiotherapy, where are you on the journey?
1. Why are you interested in content on adaptive radiotherapy?
Delivering the future of breast cancer treatment
Every breast cancer journey is different. Adaptive radiotherapy helps you tailor each treatment plan to your patient’s needs at every session. Using five-fraction schedules, you can reduce treatment time and help patients spend less time in therapy and more time living, while protecting healthy tissue and vital organs.
Adaptive workflows equip you to deliver the latest standard of care, enabling precise, efficient, and compassionate treatment for every patient.
Explore our adaptive solutions for breast cancer
Our image-guided adaptive solutions help you personalize every fraction, protecting the heart and lungs while maintaining tumor control.
References
- 2025 Global Impact Report - aboutadaptive.com (Accessed: 3 November 2025).
- Optimal Utilization rate source: GLOBOCAN; The Lancet Oncology Commission: Expanding global access to radiotherapy
- American Cancer Society. Radiation for breast cancer. Revised 10/27/2021. Available at: Radiation for Breast Cancer | Breast Cancer Treatment | American Cancer Society
- Bilski M, Konat-Baska K, Zerella MA et al. Advances in breast cancer treatment: a systematic review of preoperative SBRT for breast cancer. Radiat Oncol. 2024;19:103.
- Zabrocka E, Roberson JD, Noldner C et al. SBRT for the treatment of primary breast cancer in patients not undergoing surgery. Advan Med Sci. 2024;69(1):29-35.
- Strnad V, Polgar C, Ott OJ et al. Accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy compared with whole-breast irradiation with boost for early breast cancer: 10-year results of a GEC-ESTRO randomised, phase 3, non-inferiority trial. Lancet Oncol 2023;24(3):262-272.
- Guinot JL, Guttierrez-Miguelez, Meszaros N et al. Five-year results of the very accelerated partial breast irradiation VAPBI phase I-II GEC-ESTRO trial. Radiother Oncol 2024;201:110543
- Gaudet M, et al. Long-term results of multicatheter interstitial high-dose-rate brachytherapy for accelerated partial-breast irradiation. Brachytherapy. 2019; 18:211-216.
- Jardel P, Kammerer E, Villeneuve H et al. Stereotactic radiation therapy for breast cancer in the elderly. Transl Cancer Res. 2020;9(Suppl 1):S86-S96.
- Sager O, Dincoglan F, Demiral S et al. Adaptive radiation therapy of breast cancer by repeated imaging during irradiation. World J Radiol. 2020;12(5):68-75.
- De-Colle C, Kirby A, Russell N. Adaptive radiotherapy for breast cancer. Transl Radiat Oncol. 2022;39:100564.
- Hotsinpiller WS, Soike M, Pogue JA et al. Early clinical experience of online adaptive radiotherapy for APBI with SBRT. IJROBP. 2023;117(2)(Suppl):E181.
- Brunt AM, Haviland JS, Wheatley DA et al. FAST-Forward: one week vs three weeks. Lancet. 2020;395(10237):1613-1626.
- Brunt AM, Cafferty FY, Wheatley D et al. Five-year normal-tissue effects, nodal sub-study. Radiother Oncol. 2025;207:110915.